Central Neuropathic Pain: When the Nervous System Turns Against You


Central neuropathic pain (CNP) is a complex and often misunderstood medical condition that significantly impacts quality of life. Unlike typical pain that arises from injury to tissues such as skin, muscles, or joints, central neuropathic pain originates from damage or dysfunction within the central nervous system (CNS) — the brain and spinal cord. Because of this unique source, it presents differently, responds differently to treatment, and requires a specialized understanding for effective management.
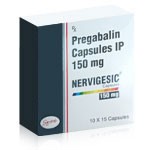
In this article, we will explore the symptoms of central neuropathic pain, its causes, how it differs from peripheral neuropathic pain, the major subtypes of neuropathic pain, available treatments, and the role of medications such as Nervigesic in therapy.
Understanding Central Neuropathic Pain
Pain perception begins when sensory nerves detect harmful or irritating stimuli and relay signals to the brain. Normally, this system serves as a protective warning. However, when the central nervous system itself is injured or altered, the signals become distorted. Instead of warning the body of real danger, the brain continues to produce sensations of pain even in the absence of ongoing injury.
This is the hallmark of central neuropathic pain: the nervous system misfires within the CNS itself, leading to persistent, chronic discomfort that can feel disproportionate to external triggers or sometimes arise spontaneously.
Symptoms of Central Neuropathic Pain
The symptoms of central neuropathic pain are varied and often distressing. Patients frequently describe unusual sensations that go beyond ordinary aching or soreness. Common symptoms include:
- Burning pain: A constant burning sensation is one of the most recognized features, often described as if the affected body part is on fire.
- Electric shock–like pain: Sudden, stabbing jolts that resemble electric currents passing through the body.
- Tingling or pins-and-needles: Persistent or intermittent prickling that can make daily activities uncomfortable.
- Allodynia: Pain from stimuli that normally should not hurt, such as light touch, clothing brushing against the skin, or even a cool breeze.
- Hyperalgesia: Exaggerated responses to painful stimuli — what might be mildly painful to most people becomes intolerable for those with CNP.
- Spontaneous pain: Pain occurring without any external stimulus at all.
These symptoms can be constant or episodic, and they may fluctuate in intensity. Beyond the physical sensations, the condition frequently contributes to fatigue, sleep disturbance, anxiety, and depression, creating a cycle that further worsens the experience of pain.
What Is the Most Common Cause of Neuropathic Pain?
Neuropathic pain, broadly defined, arises from injury or dysfunction of the nervous system. The most common cause overall is diabetes mellitus, which leads to peripheral diabetic neuropathy. High blood sugar damages peripheral nerves over time, producing burning pain and numbness, typically in the feet and legs.
Other frequent causes include post-herpetic neuralgia following shingles, chemotherapy-induced neuropathy, traumatic nerve injury, and chronic alcoholism. However, these are generally peripheral causes.
In contrast, central neuropathic pain has its own causes, which often stem from major neurological conditions such as stroke, multiple sclerosis, and spinal cord injury.
Peripheral vs. Central Neuropathic Pain
It is essential to distinguish between peripheral neuropathic pain and central neuropathic pain, as the underlying mechanisms and management strategies differ.
- Peripheral Neuropathic Pain: Originates from injury to nerves outside the brain and spinal cord — the peripheral nervous system. Examples include diabetic neuropathy, carpal tunnel syndrome, or nerve compression injuries. Symptoms usually localize to the area innervated by the damaged nerve.
- Central Neuropathic Pain: Originates from injury within the central nervous system itself—the spinal cord or brain. Examples include pain following spinal cord injury, multiple sclerosis lesions, or stroke affecting pain-processing regions. Symptoms may be more diffuse, less tied to a specific nerve territory, and harder to localize precisely.
While both forms involve faulty processing of nerve signals, central pain is typically more resistant to standard painkillers and requires different treatment strategies.
The Four Types of Neuropathic Pain
Clinicians often categorize neuropathic pain into four broad types, based on origin and clinical context:
- Peripheral Neuropathic Pain: Caused by damage to peripheral nerves, such as diabetic neuropathy or nerve entrapment.
- Central Neuropathic Pain: Resulting from damage within the brain or spinal cord, such as after a stroke or spinal cord injury.
- Mixed Neuropathic Pain: A combination of central and peripheral components, as seen in conditions like cancer pain, where tumor growth can compress peripheral nerves and simultaneously alter central processing.
- Idiopathic Neuropathic Pain: Pain without a clearly identifiable structural cause, where dysfunction of the nervous system is presumed but not pinpointed.
Recognizing the type is important because it guides therapeutic decisions and sets expectations for treatment outcomes.
Causes of Central Neuropathy
Central neuropathy develops when the central nervous system is structurally or functionally altered. Several major causes stand out:
- Stroke: One of the leading triggers, particularly when the thalamus or other sensory regions of the brain are affected. Central post-stroke pain can arise weeks to months after the vascular event.
- Multiple Sclerosis (MS): In MS, immune-mediated demyelination damages pathways in the brain and spinal cord that process sensory information, leading to chronic pain syndromes.
- Spinal Cord Injury: Trauma or compression damages ascending sensory tracts, producing pain below the level of injury.
- Tumors and Neurosurgical Procedures: Lesions or surgical interventions that disrupt sensory pathways can result in central pain.
These causes alter the delicate balance of excitatory and inhibitory signals within the CNS, leading to persistent abnormal pain signaling.
Treatment of Central Neuropathic Pain
Treating central neuropathic pain is challenging. Conventional painkillers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) usually provide little relief because they target inflammatory pain, not the altered nerve signaling that defines neuropathic pain. Instead, treatment requires a multimodal approach:
Pharmacological Approaches
- Anticonvulsants: Drugs such as pregabalin and gabapentin are first-line therapies. They stabilize nerve activity by modulating calcium channels.
- Antidepressants: Certain antidepressants, particularly serotonin-norepinephrine reuptake inhibitors (SNRIs) and tricyclic antidepressants (TCAs), are effective in modulating pain pathways.
- Topical Agents: Capsaicin patches and lidocaine plasters may help in localized cases, though their role in central pain is less established.
- Opioids: Occasionally used, though they are less effective for neuropathic pain and carry risks of dependence.
Non-Pharmacological Approaches
- Physical therapy and rehabilitation: Movement, strengthening, and stretching exercises help maintain mobility and function despite pain.
- Psychological support: Cognitive-behavioral therapy, mindfulness, and relaxation techniques address the emotional burden of chronic pain.
- Neuromodulation: Techniques like spinal cord stimulation or deep brain stimulation may be considered for refractory cases.
Because no single therapy is universally effective, treatment often involves a combination of medications and supportive measures tailored to each patient.
The Role of Nervigesic in Treatment
Nervigesic is a brand name for pregabalin, one of the most widely prescribed agents for neuropathic pain. Its role in central neuropathic pain management is particularly significant.
Pregabalin binds to the α2-δ subunit of voltage-gated calcium channels in neurons. By reducing calcium influx, it decreases the release of excitatory neurotransmitters like glutamate and substance P. This stabilizes overactive nerve circuits in the central nervous system and dampens abnormal pain signals.
For patients with central neuropathic pain — whether from spinal cord injury, multiple sclerosis, or post-stroke complications — Nervigesic has been shown to reduce pain intensity, improve sleep quality, and enhance overall quality of life. Importantly, it also helps address associated symptoms such as anxiety, which commonly coexist with chronic pain syndromes.
Dosing typically begins at a lower level and is titrated upward based on tolerance and effectiveness. While side effects such as dizziness, somnolence, or weight gain may occur, many patients find the benefits outweigh these drawbacks. Nervigesic is rarely effective alone but serves as a cornerstone around which comprehensive treatment strategies can be built.
Living with Central Neuropathic Pain
Beyond medical treatments, living with central neuropathic pain requires adaptation and resilience. Patients often benefit from structured pain management programs that combine medication, physical rehabilitation, mental health support, and lifestyle adjustments. Adequate sleep, balanced nutrition, and avoidance of alcohol or substances that exacerbate nerve dysfunction can make a meaningful difference.
Support groups and patient education empower individuals to better understand their condition and reduce the isolation that often accompanies chronic pain. Clinicians encourage realistic expectations: while complete elimination of pain is rare, substantial improvement in function and comfort is achievable.
Conclusion
Central neuropathic pain is a debilitating condition rooted in dysfunction of the central nervous system. It manifests with distinctive symptoms such as burning, tingling, and electric shock–like sensations that profoundly impair quality of life. The most common causes include stroke, multiple sclerosis, and spinal cord injury, differentiating it from peripheral neuropathic pain that arises outside the CNS.
Recognizing the four main types of neuropathic pain — peripheral, central, mixed, and idiopathic — helps clinicians tailor care appropriately. Treatment relies on anticonvulsants, antidepressants, physical and psychological therapies, and in some cases advanced neuromodulation.
Nervigesic (pregabalin) plays a central role in controlling abnormal nerve signaling and remains a first-line therapy for central neuropathic pain. Though challenging to manage, with comprehensive care patients can achieve meaningful relief and regain better quality of life.
Drug Description Sources: U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList.
Reviewed and Referenced By:
Dr. Alan Carter, PharmD Clinical pharmacist specializing in chronic pain management and antiepileptic drugs. Frequently cited on Drugs.com for reviewing therapeutic guidance on Pregabalin’s pharmacokinetics, dosage, and safety profile.
Dr. Carol DerSarkissian, MD Board-certified in internal medicine, contributor to WebMD. Her clinical reviews focus on the management of anxiety disorders and neuropathic pain. She provides expert validation on the psychiatric applications of Pregabalin.
Dr. Dianne B. McKay, MD Professor of Clinical Pharmacology, contributor to RxList and NIH. Her medical insights address the renal implications and long-term safety of antiepileptic agents like Pregabalin.
Dr. William C. Shiel Jr., MD, FACP, FACR Chief Editor at MedicineNet, affiliated with WebMD. Authored comprehensive medical content on anticonvulsants, including the mechanisms of action and known side effects of Pregabalin.
Dr. Steven Gans, MD Harvard-trained psychiatrist and senior reviewer at Verywell Mind. Provides expertise in the use of anticonvulsants such as Pregabalin for neuropathic pain and associated psychiatric conditions.
(Updated at Sep 29 / 2025)