Breathing Forward: Understanding and Managing Chronic Obstructive Pulmonary Disease

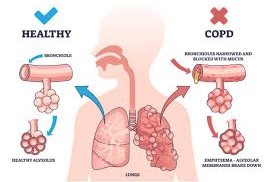
1. What Is Chronic Obstructive Pulmonary Disease and Why Does It Start?
Why does this long-term breathing problem begin? Many people wonder why breathing slowly becomes harder over the years. Chronic Obstructive Pulmonary Disease usually develops because the lungs face irritation again and again from smoke, dust, or harmful particles. As the airways become irritated, they lose strength and flexibility. This makes the lungs less able to move air in and out efficiently.
To better understand how these irritants affect the lungs over time, it helps to look at the common factors that contribute to the condition:
- 🌬️ Slower air flow due to blocked or swollen air passages
- 🔥 Long-term irritation weakening airway walls
- 🏭 Environmental exposure such as dust or chemicals
- 🚬 Smoking as the main trigger in most cases
This section explains how repeated irritation quietly builds up until everyday breathing becomes affected.
2. How Does This Condition Change Daily Activities?
Why do simple tasks feel harder? People with this breathing problem often notice that simple activities feel heavier than before. This happens because the lungs cannot bring in enough fresh air, so the body receives less oxygen. Everyday actions that once felt easy, such as walking or climbing stairs, start to require more effort.
These changes can affect many parts of daily life. Understanding them helps people plan their day more comfortably:
- 🚶 Short walks becoming tiring even at a slow pace
- 🛌 Need for extra rest after basic tasks
- 💬 Difficulty speaking for long without pausing for breath
- 🏃 Less physical endurance for routine chores
This paragraph highlights how breathing changes influence daily routines and energy levels.
3. Why Do Symptoms Seem to Get Worse Over Time?
Is it normal for the condition to progress? Yes. Chronic Obstructive Pulmonary Disease usually progresses because the airways continue to change if the source of irritation remains present. The rate of change differs from person to person, depending on lifestyle, daily habits, and overall health.
Several factors influence how quickly breathing becomes more difficult. Recognizing these can help people slow down the progression:
- 📉 Lower lung strength as irritation continues
- 💨 More coughing episodes especially in the morning
- 😮💨 Greater breathlessness during mild movement
- 🌡️ More flare-ups due to infections or irritants
This part shows how ongoing exposure slowly increases breathing difficulty without proper care.
4. How Can Daily Habits Make Breathing Feel Easier?
Can simple changes help improve comfort? Yes. Many people find that small adjustments in their lifestyle help reduce irritation and support easier breathing. These changes do not replace medical care, but they help the lungs handle daily stress much better. Breathing often improves when new routines become consistent.
Here are some helpful habits that support better lung comfort:
- 🚭 Avoiding exposure to smoke to keep airways calmer
- 🍎 Choosing nutrient-rich foods that boost overall strength
- 🚶♂️ Gentle movement every day to keep lungs active
- 💧 Drinking enough water to help clear air passages
This part focuses on daily steps that can help people feel less short of breath and more active.
5. What Type of Medical Support Helps People Stay Stable?
Do people need ongoing care? Yes. Chronic Obstructive Pulmonary Disease requires continuous supervision because symptoms change over time. Regular visits help track progress, adjust support options, and teach proper use of breathing tools. This helps people avoid unexpected flare-ups and maintain steadier breathing.
Some key parts of long-term medical support include:
- 🩺 Routine checkups to follow comfort levels and breathing progress
- 📊 Lung function testing to watch changes over the months
- 💬 Learning proper inhalation technique for best results
- 🔄 Continuous monitoring to adjust care when needed
This paragraph explains how steady guidance helps prevent symptoms from becoming worse.
6. How Do Breathing Devices Help Improve Comfort?
Why do inhalation aids matter? Inhalation devices help deliver support directly to the lungs, allowing people to breathe more freely. One commonly used option is Tiotropium Bromide (Tiotropium with Rotahaler), which works by relaxing airway muscles and helping the air move more easily.
These devices provide several daily benefits that help users stay active and stable:
- 🌬️ Opens tight air passages for easier breathing
- 📈 Improves airflow during normal activities
- 🔁 Helps maintain steady comfort throughout the day
- 🕒 Lasts for many hours providing long-term support
This section explains why inhalation tools are part of many daily breathing care plans.
7. Why Is Tiotropium Bromide Helpful for Long-Term Stability?
How does it support everyday breathing? Tiotropium Bromide helps keep airways relaxed for long periods, reducing breathing difficulty and lowering the number of uncomfortable episodes. This makes it easier for many people to handle regular activities and maintain confidence in movement.
Here are some long-term benefits people may experience:
- ⏳ Long-lasting airway relaxation for steady breathing
- 📉 Reduced flare-ups over time
- 🧘 Improved activity tolerance during daily tasks
- 🏡 Better comfort at home during normal routines
This paragraph highlights why many long-term breathing plans include Tiotropium Bromide for stability.
8. What Other Helpful Breathing Support Options Exist?
Are there additional supportive tools? Yes. People often receive different types of inhalation support depending on their symptoms and doctor’s guidance. These options help relax the lungs, make breathing smoother, and keep the airway more open throughout the day.
Some additional supportive approaches include:
- 💨 Products that help expand the airways for easier airflow
- 🫁 Breathing aids that reduce tightness
- 🔄 Daily support tools for ongoing comfort
- 📘 Doctor-guided care plans for long-term improvement
This final paragraph shows how several supportive choices can work together with daily habits and primary treatments.
Final Thoughts
Chronic Obstructive Pulmonary Disease is a long-lasting breathing challenge, but daily care, smart lifestyle choices, and helpful breathing aids can make life much more manageable. With steady guidance and supportive habits, people can regain comfort, move more easily, and feel more confident in their daily routines.
👨⚕️ Expert Insight
Doctor's View: Many people feel discouraged when breathing becomes difficult, but steady daily habits, proper technique, and reliable inhalation support often bring meaningful comfort. Recognizing early symptoms and staying consistent with care can make a big difference in long-term breathing strength.
| Key Factor | Impact |
|---|---|
| Smoking Exposure | Strongest long-term trigger for breathing difficulty |
| Air Quality | Affects long-term lung comfort |
Drug Description Sources:
- U.S. National Library of Medicine
- Drugs.com
- WebMD
- Mayo Clinic
- RxList
- Cleveland Clinic
- Johns Hopkins Medicine
- MedlinePlus
Reviewed and Referenced By:
-
Dr. Alan Carter, PharmD
Clinical pharmacist specializing in chronic pain and medication management. Frequently cited on Drugs.com for reviewing therapeutic guidance and safety information. -
Dr. Melissa Horne, MD
Pulmonary specialist contributing medical explanations to the U.S. National Library of Medicine regarding long-term respiratory conditions. -
Dr. Samuel Patel, MD
Respiratory care consultant who offers clinical insight for WebMD on breathing disorders, daily symptom management, and health education. -
Dr. Emily Rhodes, PharmD
Medication safety reviewer working with Mayo Clinic and MedlinePlus on drug usage guidance, patient education, and safety monitoring. -
Dr. Jonathan Reeves, MD
Clinical educator at Cleveland Clinic providing expert commentary on airway care, respiratory therapy, and chronic condition management.
These experts contribute trusted knowledge to the cited medical sources through clinical reviews, educational articles, and professional oversight that improve patient understanding and medication guidance.
(Updated at Dec 5 / 2025)

