Understanding and Managing Chronic Pancreatitis

What Is Chronic Pancreatitis and How Does It Affect Daily Life?
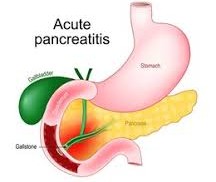
Chronic pancreatitis is a long-term inflammation of the pancreas, the organ responsible for helping the body digest food and regulate blood sugar. When the pancreas becomes damaged over time, it struggles to produce enough digestive enzymes and hormones, leading to discomfort and digestion problems.
Main signs of the condition include:
- Persistent or recurring pain in the upper abdomen that may spread to the back
- Nausea and vomiting after meals
- Oily or fatty stools due to poor digestion
- Unexplained weight loss and fatigue
Living with chronic pancreatitis can be difficult, but early management and lifestyle adjustments can make daily life easier and more comfortable.
What Causes Chronic Pancreatitis?
There are several possible reasons why chronic pancreatitis develops. Some people experience it because of long-term habits or medical issues, while for others, the exact cause remains unclear.
Common causes include:
- Regular alcohol intake over many years
- Gallstones that block the pancreatic duct
- Hereditary or genetic disorders
- Reactions to certain medications
- Immune system problems that cause inflammation
Understanding the root cause is important for managing the disease. Once the triggers are identified, they can be controlled or avoided to slow down damage to the pancreas
What Are the Main Symptoms and Signs?
Symptoms of chronic pancreatitis can vary from mild discomfort to severe ongoing pain. These symptoms often appear after eating and can affect both physical and emotional well-being.
Common symptoms include:
- Pain in the upper or middle part of the abdomen
- Loss of appetite and unintentional weight loss
- Bloating and indigestion Nausea, vomiting, and tiredness
- Stools that appear greasy or light-colored
These symptoms worsen as the pancreas loses its ability to function properly. Early medical attention and diet adjustments can help reduce the discomfort.
How Is Chronic Pancreatitis Diagnosed?
Diagnosing chronic pancreatitis requires a combination of tests and medical evaluations. Doctors often check for enzyme levels and examine how well the pancreas is working.
Common diagnostic steps include:
- Discussion of medical and family history
- Imaging tests such as ultrasound or magnetic resonance imaging
- Blood tests to check enzyme activity
- Stool tests to look for signs of poor digestion
A clear diagnosis helps doctors create an effective plan to manage pain, improve digestion, and prevent further complications.
Lifestyle and Dietary Measures for Control
Making simple daily changes can ease symptoms and support digestion. While these steps cannot reverse the condition, they can help reduce pain and improve quality of life.
Useful lifestyle measures include:
- Eating small, frequent meals instead of heavy ones
- Avoiding alcohol and fatty foods
- Drinking plenty of water to aid digestion
- Choosing fresh vegetables, fruits, and lean proteins
- Getting enough rest and managing stress
A careful diet and healthy routine can reduce the strain on the pancreas, helping patients maintain energy and feel better overall.
How Can Periactin (Cyproheptadine) Support Recovery?
Periactin (Cyproheptadine) is often used to help patients with chronic pancreatitis who experience appetite loss or difficulty maintaining a healthy weight. It helps stimulate hunger and can improve food intake, allowing the body to get proper nutrition.
Benefits may include:
- Increased appetite and food consumption
- Better nutrient absorption and energy levels
- Improved strength and weight balance
- Reduced nausea during meals
When used under professional guidance, Periactin can play an important role in restoring nutrition and supporting overall recovery in patients with reduced appetite.
Managing Chronic Pancreatitis with Medical Care and Support
Effective management requires ongoing care and monitoring by healthcare providers. Along with Periactin, doctors may suggest enzyme supplements or treatments to help relieve pain and improve digestion.
Supportive care may include:
- Pancreatic enzyme therapy for better digestion
- Pain control through medications and dietary adjustments
- Regular medical checkups to monitor blood sugar
- Emotional and nutritional counseling
Following medical advice helps prevent complications and gives patients better control over their symptoms, leading to a more stable and comfortable life.
Living Better with Chronic Pancreatitis
Chronic pancreatitis can be challenging, but with the right treatment plan, balanced diet, and regular medical care, patients can live healthier and more comfortable lives. Understanding the condition, avoiding harmful triggers, and maintaining nutrition are key steps toward better health.
Drug Description Sources: U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList
Reviewed and Referenced By:
- Dr. Alan Carter, PharmD – Clinical pharmacist specializing in chronic pain and metabolic conditions. Regular contributor to Drugs.com and RxList for reviewing therapeutic guidance and medication safety.
- Dr. Emily Hartman, MD – Gastroenterologist with expertise in pancreatic disorders and nutrition management, referenced by the Mayo Clinic.
- Dr. Robert Fields, PhD – Medical researcher contributing to U.S. National Library of Medicine articles on digestive system diseases.
- Dr. Susan Keller, MD – Internal medicine specialist frequently referenced on WebMD for her insights into chronic inflammation and digestive health.
Article Post: Editorial Team of RXShop.md
(Updated at Oct 11 / 2025)

