Early Parkinson Disease: Small Clues, Big Impact


Parkinson disease is linked to a gradual decline of dopamine-producing brain cells. Dopamine helps coordinate smooth movement, stable posture, and automatic actions (like blinking, arm swing, and facial expression). When dopamine signals weaken, the body may feel slower, stiffer, and less fluid—but the right plan can help you stay active and confident for years 😊.
Quick take 💡
Early Parkinson disease is not only about tremor. It can affect speed, stiffness, balance, sleep, mood, and energy. The best results usually come from a combination of medical care + movement + daily habits that support the brain.
🕒 When it becomes “medical”
When changes persist for weeks to months, affect daily tasks (buttons, handwriting, walking), or keep progressing, it is time for a structured evaluation—not guesswork.
🧭 What doctors check first
Symptom pattern (one side vs both), movement speed, stiffness, tremor type, posture, gait, plus sleep and mood—because early non-motor signs can appear before obvious shaking.
🎯 The real goal
The aim is stable daily function: smoother movement, safer balance, better energy, and fewer “bad days,” using a plan that evolves as your needs change.
What Is Happening in the Brain? 🧬
Parkinson disease affects movement control networks, especially circuits that rely on dopamine signaling. In early stages, dopamine reduction may be mild, and the brain can temporarily “compensate.” That is why symptoms may come and go—or show up only when you are tired, stressed, or rushing.
Over time, compensation becomes harder. Movements that used to be automatic (arm swing, facial expression, quick turns) may require extra effort. The encouraging part: movement training and timely treatment can reinforce function, even when the underlying condition is progressive.
Doctor note 👩⚕️
Dr. Irene Litvan (UC San Diego), a movement-disorders neurologist, highlights that early-stage Parkinson disease can be under-recognized because symptoms may appear subtle, variable, and easily mistaken for common “life fatigue.”
Early Signs: Motor and Non-Motor Clues 🔍
Many people expect Parkinson disease to start with shaking, but early signs can be broader. Doctors often look for a cluster of changes that build a consistent pattern.
🖐 Motor clues
- Rest tremor in one hand
- Slowness (bradykinesia): smaller handwriting, slower dressing
- Rigidity: stiffness that does not “stretch away”
- Shorter steps, less arm swing, subtle shuffling
🌙 Non-motor clues
- Sleep disruption or vivid dreams
- Constipation or slower digestion
- Lower mood, anxiety, or reduced motivation
- Reduced sense of smell
Not every symptom means Parkinson disease. But when several appear together and gradually progress, a professional assessment becomes important.
Symptoms at a Glance 📊
This table summarizes common early features and why they matter. The main idea: symptoms often start on one side, and they tend to build slowly rather than “switch on” overnight.
| Symptom | What it feels like | Why it matters |
|---|---|---|
| Resting tremor | Shaking when relaxed, improves with action | Classic early motor sign in many cases |
| Bradykinesia | Slower movements, smaller handwriting | Often the most function-limiting early sign |
| Rigidity | Stiffness, shoulder/neck tightness | Can affect posture, comfort, and gait |
| Postural changes | Stooped stance, balance uncertainty | Early safety risk, especially on turns |
Diagnosis: How Doctors Put the Pieces Together 🧩
Parkinson disease is primarily diagnosed through a detailed clinical exam and history. There is no single “one-step” lab test that confirms it. Instead, specialists look for consistent patterns: how you walk, how you turn, how fast your fingers tap, whether stiffness is present, and whether symptoms are more noticeable on one side.
Your doctor may also review medications, sleep, mood, and other conditions that can mimic Parkinson-like symptoms. In uncertain cases, additional testing may be used to rule out other causes. A careful diagnosis matters because the right label leads to the right plan.
Doctor note 👨⚕️
Dr. J. Eric Ahlskog (Mayo Clinic) emphasizes that accurate early diagnosis helps avoid unnecessary treatments and supports better long-term planning—especially when symptoms are still mild and adaptable.
Myth vs Fact 🧠✨
Myth: “No tremor = no Parkinson disease.”
Fact: Many people start with slowness, stiffness, or balance changes rather than shaking.
Myth: “Exercise can’t help the brain.”
Fact: Regular movement supports mobility, balance, and brain adaptability—especially early on.
Myth: “Treatment should wait until symptoms are severe.”
Fact: Early management can protect function and reduce future complications.
Treatment Basics: Medications + Training + Support 💊🤝
Early-stage treatment is about keeping daily life smooth and predictable. Most plans include: medication (if needed), physical activity, targeted therapy (physical/speech/occupational), and practical adjustments that reduce strain and improve safety.
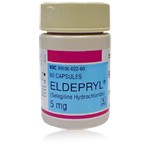
A common medication approach in early Parkinson disease involves MAO-B inhibitors. Eldepryl (Selegiline) is an MAO-B inhibitor used to treat Parkinson disease by slowing dopamine breakdown in the brain. This can support modest improvement in movement symptoms and may be especially useful when symptoms are still mild.
Doctor note 🩺
Dr. Michael S. Okun (University of Florida, Parkinson’s Foundation medical leader) often emphasizes that treatment is not only about pills— it is about building a daily routine that protects mobility, mood, and confidence over time.
Medication Strategy in Early Stage 🎯
Medication choices depend on symptom intensity, age, lifestyle, and personal goals (work, driving, hobbies). The goal is steady function, not “maximum dosing.”
| Option | What it helps | Typical role |
|---|---|---|
| MAO-B inhibitors | Modest improvement in motor symptoms | Often used early, sometimes alone |
| Dopamine agonists | Movement control via receptor stimulation | Selected patients; individualized use |
| Levodopa | Strongest symptom relief for many | Used when symptoms impact daily life |
In mild cases, Eldepryl (Selegiline) may be used as early therapy to support symptom control. In other situations, it may be combined later with additional medications as needs evolve.
What to Do First: A Practical Ladder 🪜✅
Early Parkinson disease can feel overwhelming, but the best next steps are often simple and repeatable. This ladder helps you act without turning your life into a medical project.
Step 1: Move daily 🏃♀️
Choose consistency over intensity: walking, cycling, swimming, tai chi, or strength work. Movement improves balance, gait confidence, and overall resilience.
Step 2: Train the weak links 🎯
Physical therapy can target posture, turns, and stride length. Speech therapy can strengthen voice and swallowing mechanics. Occupational therapy can keep hands efficient for daily tasks.
Step 3: Protect sleep + mood 🌙
Sleep fragmentation, anxiety, and low mood can amplify motor symptoms. Improving sleep routine and stress management often improves daily function faster than people expect.
Best principle ✅
Track progress by function: steadier walking, easier turns, better handwriting comfort, fewer “frozen” moments—small wins add up.
Why Early Treatment Can Change the Trajectory 🔄
Early Parkinson disease is a window of opportunity. The nervous system is still adaptable, routines are easier to build, and symptom patterns can be shaped with smart strategies.
Eldepryl (Selegiline) is used to treat Parkinson disease by enhancing dopamine availability through MAO-B inhibition. For selected patients, this supports smoother daily movement and may help delay the need for more intensive medication strategies. The key is personalization: what works best depends on symptoms, goals, and tolerance.
Doctor note 👨⚕️
Dr. Michael S. Okun notes that early planning—medication when appropriate, plus exercise and therapy—often produces the most “real-life” benefit: better days at work, safer walking, and more confidence in social situations.
Fast FAQ ⚡
Is early Parkinson disease always obvious?
No. Many people first notice subtle slowness, stiffness, smaller handwriting, or changes in posture—sometimes long before tremor appears.
What should I bring to a neurology visit?
A symptom timeline (when it started, what changed), a medication list, sleep notes, and a short video of tremor or gait changes if possible. Details help doctors spot patterns faster.
Can lifestyle really make a difference?
Yes. Daily movement, strength work, balance training, and sleep protection can improve function and reduce “bad-day” variability. Think of it as building a stronger “movement reserve.”
Bottom Line 🌟
Early Parkinson disease can be frightening—but it is also a stage where smart choices can have a powerful effect. With accurate diagnosis, consistent training, supportive care, and appropriate medication, many people maintain independence and a full life for years. The most important step is not perfection—it is starting.
Drug Description Sources: U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList.
Drug Description Sources: U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList.
Reviewed and Referenced By 👩⚕️👨⚕️
Dr. Michael S. Okun – Neurologist, Movement Disorders Specialist. Executive Director of the Norman Fixel Institute for Neurological Diseases at the University of Florida. Widely published in Parkinson disease research, focusing on advanced therapies, clinical management strategies, and patient-centered long-term care.
Dr. Irene Litvan – Professor of Neurosciences and Movement Disorders Specialist. Recognized for her work in early diagnosis of Parkinson disease and atypical parkinsonian syndromes, with extensive contributions to international diagnostic criteria and clinical research.
Dr. J. Eric Ahlskog – Neurologist and former Professor of Neurology at Mayo Clinic. Author and expert in Parkinson disease treatment strategies, known for translating complex neurological concepts into practical, evidence-based patient guidance.
(Updated at Feb 12 / 2026)