Management of Motor Fluctuations: A Practical Clinical Framework


Motor fluctuations mark the moment when movement control stops feeling stable and starts behaving like a switch. One part of the day feels smooth and predictable (“ON”), while another suddenly brings stiffness, slowness, tremor, or freezing (“OFF”). ⚖️ For many patients, this phase is emotionally exhausting — daily life becomes centered around timing, anticipation, and avoiding risk rather than simply living.
The purpose of management of motor fluctuations is not to eliminate every symptom, but to restore predictability. When patients know when they will move well, they regain confidence, independence, and safety. 🧭
🎯 Primary goal
Increase usable ON time while minimizing disruptive OFF periods.
⏱️ Timing matters
Consistent schedules outperform aggressive dose increases.
🍽️ Food interaction
Meal composition can delay or weaken medication response.
📊 Tracking
Simple records turn confusion into actionable patterns.
1️⃣ How Motor Fluctuations Present in Everyday Life
Motor fluctuations are rarely random. They tend to follow recognizable rhythms tied to medication timing, digestion, sleep, and stress. The challenge is that patients often describe symptoms emotionally (“bad mornings,” “terrible afternoons”), while effective management requires time-based clarity.
| Pattern | What Patients Experience | Underlying Reason |
|---|---|---|
| Wearing-off | Gradual loss of mobility before next dose | Shortened medication effect |
| Delayed ON | Medication works late or inconsistently | Slow gastric emptying or protein interference |
| Sudden ON–OFF | Abrupt loss of movement without warning | Unstable absorption or sensitivity shifts |
| Early morning OFF | Severe stiffness after waking | Insufficient overnight dopamine support |
🚨 Clinical priority: OFF periods that involve falls, freezing in doorways, or swallowing difficulty should be addressed urgently, even if total ON time seems acceptable.
2️⃣ Why Fluctuations Increase as the Disease Progresses
In early disease stages, dopamine-producing neurons buffer medication smoothly. Over time, that buffering capacity declines. The same dose now produces a sharper peak and a faster drop — experienced as motor instability. 📉
- Reduced dopamine storage in surviving neurons
- Shorter duration of benefit per dose
- Digestive variability from constipation or delayed emptying
- Sleep deprivation and stress amplifying motor symptoms
🔍 Understanding this shift is critical: increasing a single dose often worsens dyskinesia without fixing OFF time.
3️⃣ The Core Strategy: Smooth, Do Not Chase
Effective fluctuation control focuses on smoothing the dopamine curve. Instead of reacting to each OFF episode, clinicians design schedules that reduce peaks and fill valleys. 🌊
🕒 Schedule precision
Fixed dosing times train predictable motor response.
➗ Dose fractionation
Smaller, more frequent doses reduce wearing-off.
🧩 Add-on support
Adjunct therapies extend benefit without pushing peaks.
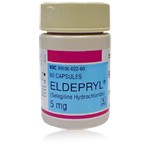
One commonly used adjunct is Eldepryl (Selegiline), a selective MAO-B inhibitor that slows dopamine breakdown and helps maintain a steadier response throughout the day.
4️⃣ Choosing Add-On Therapy Wisely
Add-on medications are not interchangeable. Each class targets a different weakness in the motor response system. Choosing correctly can reduce OFF time without adding new problems. ⚙️
| Category | Main Benefit | Key Consideration |
|---|---|---|
| MAO-B inhibitors | Prolong dopamine availability | Watch sleep and interaction profile |
| COMT inhibitors | Extend levodopa effect | May increase dyskinesia |
| Dopamine agonists | Additional stimulation | Impulse and sleep risks |
| Rescue therapies | Rapid OFF reversal | Technique-dependent |
🧠 In many patients, Eldepryl (Selegiline) fits well when OFF periods are frequent but dose escalation is poorly tolerated.
5️⃣ Practical Role of Eldepryl (Selegiline)
Eldepryl (Selegiline) works by selectively inhibiting monoamine oxidase-B, reducing dopamine degradation in the brain. Its clinical value lies in stabilization rather than stimulation.
- ⏳ Extends ON time without sharp peaks
- 🔄 Smooths transitions between doses
- 🌅 Improves morning mobility in some patients
✅ Best mindset: Use to reinforce consistency — not to chase immediate symptom relief.
6️⃣ Food, Protein, and Delayed ON
Delayed ON is often misunderstood as medication failure. In reality, it frequently reflects digestive and dietary factors. 🥗
✅ Helpful habits
- Consistent meal timing
- Address constipation proactively
- Discuss protein redistribution if needed
⛔ Common mistakes
- Heavy protein before dosing
- Irregular dose timing
- Ignoring hydration
7️⃣ Dyskinesia: When Peaks Become the Problem
Dyskinesia reflects excessive dopaminergic peaks. Increasing a dose may improve OFF time but worsen overall function. ⚠️ Management focuses on lowering peaks while protecting valleys.
- 🔽 Reduce single-dose size
- 🔁 Increase dosing frequency if appropriate
- 🔧 Adjust adjunct medications carefully
8️⃣ Simple Tracking That Makes a Difference
Even short-term tracking provides clarity. A 7–10 day diary often reveals timing errors invisible during clinic visits. 📒
| Record | Example | Purpose |
|---|---|---|
| Dose time | 08:00 / 12:00 | Identify consistency |
| ON start | 08:40 | Measure delayed ON |
| OFF start | 11:15 | Measure wearing-off |
9️⃣ When Fluctuations Become Complex
Frequent freezing, falls, or unpredictable OFF periods require specialist reassessment. At this stage, safety and independence take priority over fine motor optimization. 🛡️
Eldepryl (Selegiline) may remain part of the strategy, but advanced plans often combine multiple adjustments and closer monitoring.
🔑 Key Takeaways
- Motor fluctuations follow patterns
- Consistency often beats higher doses
- Smooth curves reduce risk and stress
- Adjuncts work best when matched to the problem
Drug Description Sources: U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList.
Reviewed and Referenced By:
- Dr. Michael S. Okun, MD — Board-Certified Neurologist; Movement Disorders Specialist; Director, Norman Fixel Institute for Neurological Diseases.
- Dr. Rajesh Pahwa, MD — Professor of Neurology; Director, Parkinson Foundation Center of Excellence.
- Dr. Irene H. Richard, MD — Associate Professor of Neurology and Psychiatry; Movement Disorders Researcher.
(Updated at Jan 16 / 2026)