Ankylosing Spondylitis: Causes, Symptoms, Diagnosis, and Treatment
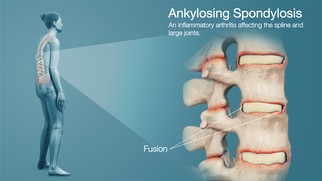
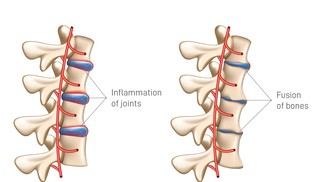
Ankylosing spondylitis (AS) is a chronic inflammatory disorder primarily affecting the spine and the sacroiliac joints at the base of the spine. Over time, this inflammation can lead to new bone formation and fusion of the vertebrae, resulting in a rigid spine. While AS is often perceived as a back disease, its systemic nature means it can also affect the eyes, lungs, heart, and even gastrointestinal system in severe cases.
The Root of the Condition: What Causes Ankylosing Spondylitis?
Though the precise cause of AS remains unknown, there is strong evidence that genetics play a pivotal role. The most significant link is with the HLA-B27 gene, found in more than 90% of patients with AS in Western populations. However, it's important to note that only a small percentage of people with this gene actually go on to develop the condition. This suggests that environmental triggers such as bacterial infections or immune system abnormalities may interact with genetic predisposition to initiate the disease.
Additional studies have proposed that changes in the gut microbiota may contribute to the onset or progression of AS. These alterations might provoke immune responses that extend beyond the intestines and into the joints and spine, driving inflammation.
Key Symptoms: Recognizing the Early Signs
The clinical presentation of ankylosing spondylitis often starts subtly, which can lead to delays in diagnosis. Typically, the first symptom is inflammatory back pain. Unlike mechanical back pain that improves with rest, inflammatory back pain improves with physical activity and worsens during inactivity or at night. This pain is usually accompanied by significant morning stiffness lasting more than 30 minutes.
As the disease progresses, fusion of the spinal vertebrae may occur, limiting mobility and causing a characteristic stooped posture. Other joints, including the shoulders, hips, and knees, may also become involved.
Eye inflammation, specifically anterior uveitis, is a well-known extra-articular manifestation, causing redness, pain, and blurred vision. Gastrointestinal symptoms, fatigue, and weight loss may also occur, particularly in cases overlapping with inflammatory bowel disease.
Is Ankylosing Spondylitis a Lifelong Condition?
Yes, AS is a lifelong disease. However, it presents on a spectrum—from mild cases with infrequent flares to severe forms that lead to extensive spinal fusion and functional impairment. Importantly, with the advancement of modern therapies and early interventions, the disease course can often be significantly altered.
The permanence of the disease doesn't imply a uniformly poor prognosis. With early detection, regular follow-ups, and tailored therapy, many patients can lead full, active lives with manageable symptoms. The chronic nature of AS does demand ongoing attention to physical health, mental well-being, and social support.
Diagnosis: Tools and Tests
Diagnosing AS is not always straightforward. It relies heavily on a combination of patient history, physical examination, imaging techniques, and lab tests.
Patients often report a slow onset of back pain before the age of 40, morning stiffness, and improvement with exercise. During physical exams, limited spinal mobility, positive Schober test, and reduced chest expansion may be observed.
Imaging plays a crucial role. Conventional radiography (X-rays) can reveal sacroiliitis — changes in the sacroiliac joints — but these changes may take years to become visible. Magnetic resonance imaging (MRI) allows for earlier detection by identifying active inflammation.
Blood tests include inflammatory markers like ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein). A positive HLA-B27 test supports the diagnosis but is not solely determinative.
Life Expectancy and Quality of Life
Generally, life expectancy in people with ankylosing spondylitis is only slightly reduced, if at all. Most patients live a normal lifespan. That said, those with severe disease may face higher risks of complications — particularly cardiovascular disease due to chronic systemic inflammation.
Functional disability may arise from spinal fusion, leading to reduced lung capacity and limited physical mobility. These risks underline the importance of comprehensive disease management, including cardiovascular monitoring and respiratory exercises.
Mental health also plays a critical role. Chronic pain, fatigue, and physical limitations can lead to depression or anxiety. Mental health support and counseling are therefore key elements of care.
Indocin (Indomethacin): A Pillar of Symptom Control
Indocin, or indomethacin, remains one of the most effective NSAIDs (non-steroidal anti-inflammatory drugs) for AS. Its potent anti-inflammatory properties help relieve pain and stiffness, especially in the early stages. For many patients, daily use of Indocin significantly improves quality of life by allowing better mobility and reduced discomfort.
Despite its effectiveness, long-term use of Indocin must be monitored closely. Potential side effects include gastrointestinal ulcers, kidney damage, and elevated blood pressure. Patients are often advised to take it with food and to undergo routine evaluations to assess for complications.
In some cases, when NSAIDs alone are insufficient, treatment may escalate to include biologics such as TNF inhibitors (e.g., adalimumab, infliximab) or IL-17 inhibitors (e.g., secukinumab). These advanced therapies target the underlying immune pathways driving the disease and can significantly reduce disease activity.
Living with Ankylosing Spondylitis: A Holistic Approach
Optimal management of AS is multidisciplinary. Rheumatologists, physiotherapists, primary care providers, and even ophthalmologists (for eye involvement) may all be part of a patient’s care team.
Daily physical activity is essential — not only to maintain spinal flexibility but also to support cardiovascular health and combat fatigue. Stretching exercises, posture training, and swimming are particularly beneficial. In more advanced stages, assistive devices or orthopedic consultations may be necessary.
Nutrition also plays a supporting role. While no specific diet cures AS, a balanced, anti-inflammatory diet rich in omega-3 fatty acids, whole grains, and fresh vegetables may help manage symptoms. Some patients report improvement with gluten-free or low-starch diets, although more research is needed in this area.
In summary, ankylosing spondylitis is a multifaceted and lifelong condition, but one that can be managed effectively with early diagnosis and comprehensive care. With medications like Indocin, physical therapy, and lifestyle adjustments, patients can preserve their mobility and lead full, independent lives.
Article Post:Editorial Team of RXShop.md
(Updated at Apr 14 / 2025)