Understanding and Managing Opioid Withdrawal Syndrome

What Is Opioid Withdrawal Syndrome and Why Does It Happen?
Have you or someone you know ever tried to stop using opioids and experienced intense physical or emotional discomfort?
The likely explanation is a condition known as Opioid Withdrawal Syndrome (OWS)—a collection of symptoms that occur when a person reduces or stops using opioid drugs after prolonged use.
- Opioids like heroin, oxycodone, morphine, and fentanyl change the way the brain and body perceive pain and pleasure.
- Long-term use of opioids leads to physical dependence, meaning the body adapts to their presence.
- When opioids are no longer taken, the body reacts with withdrawal symptoms, as it struggles to adjust.
- OWS is not just unpleasant—it can be dangerous if not managed properly.
Understanding this condition is essential in helping individuals recover safely from opioid addiction. Recognizing the signs and knowing the treatment options makes recovery more achievable.
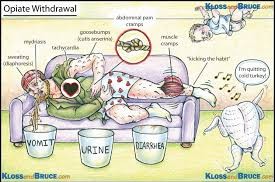
Recognizing the Symptoms of Opioid Withdrawal Syndrome
The symptoms of OWS can range from uncomfortable to severe, often pushing individuals back into drug use just to stop the pain.
Early symptoms include:
- Anxiety and agitation
- Muscle aches
- Sweating
- Runny nose and watery eyes
- Yawning frequently
Later symptoms include:
- Nausea and vomiting
- Abdominal cramping
- Diarrhea
- Dilated pupils
- Goosebumps and chills
These symptoms can begin within 6-12 hours of the last dose of a short-acting opioid, or within 30 hours for longer-acting opioids like methadone. The severity varies depending on the level of dependence and the specific opioid used.
Risk Factors That Worsen Opioid Withdrawal
Not everyone experiences withdrawal the same way. Several factors influence the intensity and duration of symptoms.
Key risk factors include:
- Length and intensity of opioid use – The longer and more frequently opioids are used, the stronger the withdrawal.
- Type of opioid – Some opioids, such as heroin, may cause more intense symptoms.
- Co-occurring mental health conditions – Anxiety, depression, and trauma can increase withdrawal discomfort.
- Polysubstance use – Mixing opioids with other substances (alcohol, benzodiazepines) complicates withdrawal.
- Lack of medical support – Going "cold turkey" without medical help can make symptoms unbearable and dangerous.
Understanding these risk factors helps in planning effective, individualized treatment strategies.
Medical and Non-Medical Approaches to Managing Withdrawal
Managing opioid withdrawal requires a structured approach. Without assistance, the process is extremely difficult.
Medical treatment options include:
- Medications such as buprenorphine or methadone to ease withdrawal symptoms
- Symptom-targeted treatments, like anti-nausea or anti-diarrheal drugs
- Supervised detox programs that monitor vitals and provide safety
Non-medical strategies include:
- Hydration and nutrition support
- Rest and a calm environment
- Counseling and emotional support
- Mindfulness or breathing exercises
Treatment should be personalized. What works for one person may not work for another, which is why professional guidance is crucial.
The Role of Catapres (Clonidine) in Opioid Withdrawal
Among the most effective non-opioid medications used to manage withdrawal is Catapres, also known as Clonidine.
How Catapres helps:
- Reduces anxiety, sweating, runny nose, and muscle aches
- Helps lower blood pressure and heart rate, calming the nervous system
- Does not produce a "high," making it non-addictive
- Can be used alone or alongside other medications during withdrawal
Clonidine doesn't eliminate all withdrawal symptoms but makes the process more tolerable, especially when combined with emotional support and a recovery plan. It is often prescribed in outpatient settings and can be a powerful tool in easing early withdrawal symptoms safely. Overcoming opioid withdrawal is the first step toward a drug-free life. While the road is challenging, support, medical care, and the right medications—such as Catapres—can make a significant difference. The key is recognizing the problem, understanding its symptoms and risks, and seeking appropriate treatment. Recovery is possible, and every step toward managing withdrawal is a step closer to reclaiming life.
Article Post: Editorial Team of RXShop.md
(Updated at May 10 / 2025)