Living with Bipolar Disorder


Bipolar disorder is a complex mental health condition that affects mood, energy, and daily functioning. It is characterized by extreme mood shifts that include periods of elevated mood, known as mania or hypomania, and episodes of depression. Unlike typical changes in mood that most people experience, these shifts are intense, disruptive, and can last for weeks or even months. Bipolar disorder does not define a person’s intelligence, creativity, or capabilities, but it does present challenges that often require lifelong management through therapy, lifestyle adjustments, and medication.
What Bipolar Disorder Really Means
At its core, bipolar disorder involves an imbalance in brain chemistry and neural pathways that regulate mood and emotions. The disorder is thought to result from a combination of genetic, biological, and environmental factors. Families with a history of bipolar disorder or severe depression may carry a higher risk, while stressful life events, trauma, or substance abuse can sometimes trigger its onset. The illness is chronic, meaning it persists across a lifetime, but its intensity and expression vary from person to person. Some individuals may experience long stretches of stability, while others cycle more frequently between manic and depressive states.
Bipolar disorder is typically divided into different types. Bipolar I involves full manic episodes often severe enough to require hospitalization, alternating with major depressive episodes. Bipolar II is defined by hypomanic episodes that are less extreme but still disruptive, along with prolonged depressive episodes. Cyclothymic disorder, a milder form, includes fluctuating low-level hypomania and depression that persist over long periods. Despite these distinctions, all forms share the hallmark of dramatic mood instability.
Recognizing the Signs
Because bipolar disorder affects both ends of the emotional spectrum, its symptoms differ depending on whether a person is experiencing mania or depression. During manic phases, individuals may feel an overwhelming surge of energy and euphoria. They might sleep very little, talk rapidly, or engage in impulsive behaviors such as spending sprees or risky ventures. Thoughts can race so quickly that it becomes difficult to focus or maintain coherent conversations. On the other end, depressive episodes bring profound sadness, fatigue, hopelessness, and sometimes thoughts of death or suicide.
Clinicians often point to a few key signs that strongly suggest the presence of bipolar disorder. These include unusually elevated mood and energy, erratic sleep patterns without feeling tired, impulsive decisions with potential negative consequences, prolonged periods of sadness or withdrawal, and noticeable changes in thinking or concentration. When these patterns appear recurrently and disrupt work, school, or relationships, they are more than ordinary mood fluctuations — they indicate a medical condition that requires attention.
Life with Bipolar Disorder
A common question for individuals receiving a diagnosis is whether it is possible to lead a normal life. The answer, supported by decades of research and countless personal stories, is yes. With proper treatment, many people with bipolar disorder achieve stability and pursue fulfilling careers, relationships, and goals. The key lies in recognizing triggers, adhering to treatment plans, and maintaining support networks.
Successful management often includes therapy sessions that teach coping strategies, stress management, and emotional regulation. Cognitive behavioral therapy and psychoeducation have proven especially useful, as they help patients understand their condition and anticipate mood changes. Daily routines play a significant role as well — consistent sleep, exercise, and structured activities can stabilize mood. Support groups and close relationships provide an additional safety net during vulnerable times.
However, the road is rarely linear. Relapses and setbacks may occur, especially when medications are adjusted or during stressful life events. But these episodes do not negate progress. Instead, they remind patients and families that bipolar disorder, much like diabetes or heart disease, is a condition requiring lifelong vigilance and self-care. With resilience and ongoing treatment, stability and happiness remain attainable.
The Human Side of Bipolar Disorder
Understanding what a bipolar person is like requires nuance. Stereotypes often paint them as unpredictable or dangerous, but in reality, they are individuals with unique personalities, talents, and values who happen to live with a medical condition. During stable periods, many are indistinguishable from those without the diagnosis. They work, parent, create art, manage businesses, and contribute to society in countless ways.
When mood episodes occur, their behaviors may differ sharply from their baseline. In mania, some may appear overly confident, restless, or irritable. They might pursue multiple projects with enthusiasm but without follow-through. In depression, they can seem withdrawn, disinterested, or pessimistic. Importantly, these are not permanent states but symptoms of an illness. Recognizing the distinction between the person and the condition is essential for reducing stigma and supporting recovery.
Many people with bipolar disorder describe their experience as a double-edged sword. The high energy of hypomania can fuel creativity and productivity, while the depths of depression can foster empathy and introspection. The challenge is to harness the positive aspects while minimizing the risks and suffering. With compassion and awareness, friends and family can provide invaluable support by encouraging treatment, listening without judgment, and offering stability during turbulent times.
Treatment Approaches
The treatment of bipolar disorder is multifaceted. Medications form the backbone of therapy, complemented by counseling and lifestyle strategies. Mood stabilizers such as lithium remain a cornerstone, while anticonvulsants and certain atypical antipsychotics are commonly prescribed. These medications aim to prevent extreme highs and lows, reducing the frequency and severity of episodes.
Psychotherapy plays an equally critical role. Therapy helps patients identify early warning signs, navigate relationship challenges, and adhere to medication plans. It also offers a safe space to process the psychological impact of living with a chronic illness. Family involvement often strengthens outcomes, as education and communication reduce misunderstandings and conflicts.
Healthy habits — balanced diet, regular physical activity, and adequate rest—also reinforce stability. Because substance abuse can worsen symptoms, avoiding alcohol and drugs is strongly advised. Ultimately, successful treatment is personalized, requiring ongoing communication between patient and healthcare provider.
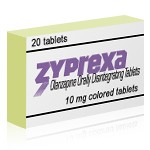
The Role of Zyprexa
Among the medications used for bipolar disorder, Zyprexa (olanzapine) occupies an important place. It is an atypical antipsychotic initially developed to treat schizophrenia but later found effective in managing bipolar disorder. Zyprexa helps by influencing neurotransmitters such as dopamine and serotonin, which are key players in regulating mood and thought processes.
Zyprexa is particularly valuable during acute manic episodes. It reduces agitation, racing thoughts, and excessive activity, allowing individuals to regain a sense of calm and control. For some, it is also prescribed alongside mood stabilizers or antidepressants to maintain long-term balance. Its sedative properties can help normalize sleep, which is often disrupted during mania. Clinical studies demonstrate that patients on Zyprexa often experience fewer relapses and more stable mood cycles.
However, like all medications, Zyprexa carries potential side effects. Weight gain, drowsiness, metabolic changes, and increased appetite are commonly reported. Because these effects can increase the risk of diabetes and cardiovascular issues, doctors monitor patients closely with regular check-ups and blood tests. The decision to use Zyprexa is based on weighing the benefits of mood stabilization against these risks. For many, the positive impact on quality of life outweighs the drawbacks, especially when combined with healthy lifestyle habits to mitigate side effects.
Living with Hope
Although bipolar disorder can feel overwhelming, it is not a sentence to a diminished life. Advances in medicine, increased awareness, and growing social support make it more manageable today than ever before. Celebrities, writers, scientists, and everyday people openly share their stories, breaking down stigma and proving that success and stability are possible.
Education is one of the strongest tools in combating fear and misinformation. Understanding that bipolar disorder is a medical condition — not a flaw or weakness — shifts the conversation from blame to support. Employers, schools, and communities can contribute by fostering inclusive environments that accommodate mental health needs. On an individual level, self-compassion and patience are vital. Learning to accept limitations while celebrating achievements helps create balance.
With consistent treatment, open communication, and resilience, many people with bipolar disorder not only live normal lives but also thrive. They develop deep empathy, creativity, and perseverance — qualities that enrich both their own lives and the world around them. Zyprexa and other modern therapies provide powerful tools, but hope, understanding, and human connection remain the strongest allies in the journey toward wellness.
Drug Description Sources:
U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList.
Reviewed and Referenced By:
Dr. Trisha Suppes, MD, PhD Professor of Psychiatry, Stanford University. Director of the Bipolar and Depression Research Program. Recognized expert in the biological basis and long-term management of bipolar disorder.
Dr. Ellen Leibenluft, MD Senior Investigator, National Institute of Mental Health (NIMH). Her research focuses on the neuroscience and developmental aspects of mood dysregulation and bipolar disorder, including irritability in children.
Dr. Mauricio Tohen, MD, DrPH Distinguished Professor and Chair of Psychiatry & Behavioral Sciences at the University of New Mexico. Known for leadership in clinical trials and treatment outcome research in bipolar and psychotic disorders, including the use of olanzapine in maintenance therapy.
Dr. Dost Öngür, MD Chief of the Psychotic Disorders Division at McLean Hospital and Professor at Harvard Medical School. A prolific researcher in mood disorders and neuroimaging, with numerous publications addressing the pathophysiology and treatment of bipolar disorder.
(Updated at Oct 2 / 2025)