Painful Muscle Spasms – When the Body Locks Instead of Moves


😣 Painful muscle spasms are not “just cramps.” They are sudden bursts of involuntary contraction that can clamp a muscle so tightly it feels locked, twisted, or squeezed. One spasm can be over in seconds — but the soreness, stiffness, and “don’t-move-or-it-will-happen-again” fear can last for hours. The reason is simple: spasms often involve nerve signaling (the command system), not only the muscle tissue (the engine).
🧠 The spasm–pain loop (why it keeps coming back)
When a muscle stays contracted, blood flow drops and oxygen delivery falls. Metabolic byproducts build up and irritate nerve endings. The brain interprets that irritation as danger and raises sensitivity — which makes the next spasm easier to trigger. That creates a classic feedback loop 🔁:
- Trigger → posture, overuse, stress, dehydration, nerve irritation
- Contraction → muscle locks and compresses local circulation
- Chemical irritation → pain receptors fire more intensely
- Nerve sensitization → the system becomes “jumpier”
- Repeat → smaller triggers cause bigger spasms
Doctor note 👩⚕️
If your muscle “jumps” at light touch or spasms appear with minimal movement, it often signals a sensitized nervous system. In that case, calming the system usually works better than forcing aggressive stretching.
✅ The 10-second goal
Confirm what is spasming, why it’s happening, and what your plan is (so you don’t treat guesses).
📍 Location matters
Calf cramps, back “lockups,” and neurologic limb stiffness often have different causes and need different strategies.
🛠️ Technique matters
Gentle + consistent beats intense + rare. With spasms, “more force” often equals more guarding.
⏳ Patience matters
Most outcomes are judged over weeks, not days. The nervous system needs repetition to calm.
🔍 What triggers spasms (spot your pattern)
Many spasms look random — until you track them. Common triggers include:
- 💧 Dehydration or sweating without fluid replacement
- 🧂 Electrolyte shifts (magnesium/potassium changes, diuretics)
- 🪑 Long sitting and compressed posture (hip flexors/back tightening)
- 🏋️ Overuse or sudden load spikes (weekend workouts, heavy lifting)
- ⚡ Nerve irritation (disc issues, sciatica, spinal stenosis)
- 😮💨 Stress + poor sleep (higher muscle tone and lower pain threshold)
Quick win: If you can find the trigger category, your plan becomes more precise and your progress becomes faster.
🗺️ Quick symptom map (what your spasm is trying to tell you)
| Spasm pattern | Common driver | What usually helps most |
|---|---|---|
| Night calf/foot cramps 🌙 | Fluid/electrolyte shifts, fatigue, circulation factors | Hydration routine, gentle stretch, regular walking |
| Back “locks up” after bending | Protective guarding around irritated structures | Heat, graded movement, posture reset, micro-breaks |
| Spasm + tingling or shooting pain ⚡ | Nerve compression/irritation | Reduce nerve irritation, gentle core stability, avoid flare movements |
| Persistent stiffness with jerky release | Neurologic spasticity pattern | Rehab + spasticity-focused medical plan |
📋 Step 1 — Confirm the problem (do not treat guesses)
The biggest reason people fail to improve is not effort — it’s treating the wrong driver. Spasms can mimic many conditions (strain, nerve pain, spasticity, circulation issues). If the pattern is unclear, start with a safe, low-intensity plan and confirm what you’re dealing with.
Doctor note 👩⚕️
If pain is escalating quickly, comes after injury, or is paired with new neurologic changes, confirmation is more important than speed. A short check can prevent weeks of frustration.
🧾 Step 2 — What to tell your doctor (high-impact checklist)
- Exact location (calf, back, shoulder, thigh) and whether pain radiates
- Timing (night, after sitting, after exercise, during stress)
- Frequency (daily? weekly? clusters?) and typical duration
- Neurologic clues (numbness, tingling, weakness, balance changes)
- Medication and supplements (diuretics, statins, stimulants, magnesium)
- Hydration + sleep quality (both strongly affect spasm threshold)
- Functional impact (walking distance, sleep disruption, work limits)
🧠 Step 3 — Self-check before you “push through”
Use this quick check. If you hit red flags, it’s safer to pause and get guidance.
✅ Green light
- Spasms improve with gentle warmth and slow movement
- No progressive weakness or numbness
- You can walk and function between episodes
- Clear trigger (overuse/posture/dehydration)
⚠️ Yellow flags
- Spasms wake you often or cluster repeatedly
- Pain radiates or tingling appears intermittently
- Spasms worsen after stretching harder
- You’re starting new meds that affect hydration or nerves
🛑 Red flags — pause and seek care
- New or worsening weakness (foot drop, grip loss)
- Severe swelling, redness, warmth in one limb
- Fever or unexplained systemic illness with spasms
- Major trauma or inability to bear weight
- New bladder/bowel changes
⚖️ Quick comparison — start now vs wait for confirmation
Sometimes waiting a few days for confirmation prevents weeks of unnecessary pain. Choose the lane that matches your situation:
✅ Start now (when appropriate)
- Trigger is clear (overuse, posture, dehydration)
- No red-flag symptoms
- You can follow a consistent routine for 10–14 days
- Symptoms ease with gentle warmth and controlled movement
🕵️ Wait and confirm (often smarter)
- Diagnosis is uncertain or symptoms are atypical
- Neurologic signs are present (weakness/numbness)
- Spasms are escalating or disabling sleep repeatedly
- You suspect a nerve compression problem
Clinical perspective 🩺
The strongest outcomes usually come from precision: correct driver + consistent routine + early adjustment when the pattern is not improving.
🪜 Step-by-step routine — small steps that prevent big flare-ups
This is a practical routine you can actually repeat (and repetition is the point). Keep it gentle, consistent, and track your response.
🎯 Target
Identify the exact muscle group that spasms most often (calf, hamstring, low back). Precision beats “stretch everything.”
🧴 Warm-up
Use warmth (shower or warm pack) 5–10 minutes if tolerated. Warm tissue is less reactive.
🧘 Stretch
Stretch to mild tension, not pain. Hold 20–30 seconds, repeat 2–3 times. Avoid bouncing.
🚶 Re-train
After stretching, do 3–5 minutes of easy movement (walk, gentle range-of-motion) to “teach” the new length.
- Micro-break rule 🪑: if you sit a lot, stand and move for 60–90 seconds every 30–45 minutes.
- Hydration cue 💧: if spasms happen at night, review your evening hydration pattern (without overdoing it).
- Load rule 🏋️: reduce intensity, increase frequency (shorter sessions more often).
- Breathing reset 🌬️: slow exhale lowers nervous system arousal and can reduce spasm threshold.
Practical comfort tip ✅
Friction and compression can keep muscles “on edge.” Many people improve simply by switching to looser clothing, avoiding tight waistbands, and adjusting seating so hips and spine aren’t locked in one position.
⏱️ Typical timing patterns (what improvement usually looks like)
People expect linear progress. Spasm recovery is often staged. The nervous system calms first, then the muscle gradually becomes less reactive.
- 🌱 Early responders: fewer spasms within 3–7 days when triggers are controlled consistently.
- 🪴 Delayed responders: stiffness improves first, pain improves later; the “last mile” may take 2–4 weeks.
- 🌿 Mixed responders: one region improves quickly while another (back/hip) lags due to posture and load habits.
Goal: fewer episodes + lower intensity + better sleep. One perfect day is nice — but the real win is a better weekly trend.
⚖️ Benefits vs side effects (how to interpret your response)
You want a response that is noticeable but manageable. If your plan helps spasms but makes you nonfunctional, it needs adjustment.
Good balance ✅
Spasms are less frequent, muscles feel looser, sleep improves, and you can still do normal activities.
Too much 🛑
Marked dizziness, heavy sedation, or low-blood-pressure symptoms interfering with daily function. That usually means reassessment is needed.
Clinical perspective 🩺
The best plan is the one you can follow consistently. Consistency beats intensity — especially with spasm-prone systems.
💊 Where medication can fit (a functional goal, not a knockout)
Medication is most useful when spasms are frequent, disrupt sleep, block rehabilitation progress, or keep triggering protective guarding. The goal is to create a “window” where you can move normally again — then use that window to rebuild stability.
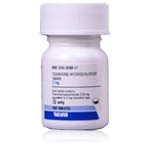
Zanaflex (Tizanidine) is a centrally acting muscle relaxant used to reduce spasticity and painful muscle tightness by calming excessive nerve signaling. When that signal “volume” drops, muscles can release, pain eases, and stretching becomes more productive instead of provoking.
- 🎯 Best use case: recurrent spasms that keep returning despite trigger control and gentle rehab.
- ✅ What success looks like: fewer lock-ups, improved sleep, better tolerance for movement.
- 🚫 What you should not aim for: being overly sedated. The target is relief with function.
📒 Patient observation log (helps you and your clinician)
A simple log turns vague discomfort into clear patterns. Track these three things for 10–14 days:
Patient note 🧾
I track: (1) spasm count per day, (2) pain level 0–10, (3) what happened right before the spasm (posture, activity, stress, hydration). If pain jumps above my normal tolerance or I notice red-flag symptoms, I pause and contact a clinician instead of pushing through.
- 🗓️ Record the day and timing (morning/night)
- 📌 Note triggers (sitting long, workout, dehydration, stress)
- 🧊 Note what helped (warmth, short walk, gentle stretch)
- 🛑 Write down stop-signs (weakness, swelling, fever, unusual symptoms)
| What you record | Why it matters | How it changes your plan |
|---|---|---|
| Time of day | Night spasms often reflect sleep/hydration drivers | Adjust evening routine + add gentle mobility |
| Posture before spasm | Static posture increases guarding | Use micro-break schedule + seating adjustments |
| Load spikes | Overuse increases excitability | Reduce intensity; increase frequency |
🧩 Special situations (caution without panic)
Some people are more sensitive to spasms or to the side effects of therapies. A structured plan helps you stay safe and consistent.
🤰 Pregnancy
New or severe cramps should be assessed. Avoid self-directed aggressive dosing changes and confirm the safest plan with a clinician.
🍼 Breastfeeding
Discuss any medication plan with your clinician, and prioritize non-drug strategies when possible.
🛡️ Immune or chronic conditions
When multiple conditions overlap, response can be unpredictable. Follow-up and confirmation are higher priority.
👵 Older adults
Sensitivity to dizziness and sedation may be higher. Structured pacing and careful monitoring are essential.
🧠 Clinical perspective — the best first move is precision
From a practical standpoint, the best way to improve outcomes is not to “push harder.” It is to start with precision: confirm the driver, choose a plan you can follow, and adjust early if the trend is not improving. If you begin accurately, you usually need fewer resets, see clearer progress patterns, and regain function faster.
🧷 Medication safety basics (simple, high-value)
If medication is part of the plan, aim for symptom control without losing daily function. Start low, adjust carefully, and avoid stacking multiple sedating agents unless guided by a clinician.
Zanaflex (Tizanidine) is commonly introduced with gradual adjustment to balance benefit and tolerability. During dose changes, use extra caution with driving and alcohol, and report excessive dizziness or heavy sedation so the plan can be tuned.
Drug Description Sources: U.S. National Library of Medicine, Drugs.com, WebMD, Mayo Clinic, RxList.
Reviewed and Referenced By:
Dr. Kalina Sanders, MD – Neurologist, Fellowship in Multiple Sclerosis and Neuroimmunology. Clinical focus on spasticity, neuromuscular disorders, and central nervous system–driven muscle dysfunction.
Dr. Zachary Bohart, MD – Board-Certified Physiatrist (Physical Medicine and Rehabilitation). Specializes in chronic pain, musculoskeletal disorders, and functional recovery in patients with muscle spasticity and movement limitations.
Dr. Andrea J. Boon, MD – Professor of Physical Medicine and Rehabilitation and Electrodiagnostic Medicine. Internationally recognized specialist in neuromuscular disease, spasticity management, and rehabilitation medicine.
(Updated at Jan 15 / 2026)