Chronic Fatigue: Understanding, Living With, and Managing the Condition


Chronic fatigue is a deeply misunderstood and often underestimated medical condition. Unlike ordinary tiredness, which can usually be resolved with rest, chronic fatigue persists for months or even years, significantly impacting a person's quality of life. Known medically as Chronic Fatigue Syndrome (CFS) or Myalgic Encephalomyelitis (ME), this condition affects millions worldwide, cutting across all demographics and often leaving sufferers feeling isolated and frustrated.
What Does Chronic Fatigue Feel Like?
For those who have never experienced chronic fatigue, it can be difficult to understand the depth and pervasiveness of the exhaustion. It is not simply being "very tired" after a long day or a bad night's sleep. Chronic fatigue feels like a profound, unrelenting exhaustion that is not relieved by rest or sleep. It often comes with a constellation of other symptoms, including muscle and joint pain, headaches, impaired memory or concentration (sometimes referred to as "brain fog"), sore throat, and enlarged lymph nodes.
This exhaustion can be so severe that everyday tasks become monumental challenges. Something as simple as taking a shower or preparing a meal can require careful planning and recovery time. Many patients describe feeling like their body is weighed down, as if gravity has intensified. Emotional stress and physical exertion often exacerbate symptoms, leading to "crashes" where functionality is severely reduced for days or weeks.
Am I Fatigued or Just Lazy?
One of the most insidious aspects of chronic fatigue is the internal doubt and guilt it can generate. Many patients struggle with the question, "Am I fatigued or just lazy?" It is important to make a clear distinction. Laziness implies an unwillingness to act despite having the physical and mental energy to do so. Chronic fatigue, by contrast, represents a genuine and debilitating physical inability to function.
Scientific research has demonstrated biological abnormalities in patients with CFS, including immune system dysfunction, neuroinflammation, and abnormalities in energy metabolism. These are not markers of laziness but indicators of a serious medical disorder. Recognizing this distinction is crucial for both patients and those around them. It validates the suffering and challenges faced daily by individuals with CFS and promotes a more compassionate and supportive approach to care.
Can You Live a Normal Life With CFS?
Living a "normal" life with CFS depends heavily on the severity of the condition and the individual's ability to manage their symptoms. For many, CFS necessitates significant adjustments to daily routines, career ambitions, and social activities. Full-time work may become impossible, and social relationships can be strained due to the unpredictable nature of the illness.
However, many patients find ways to live fulfilling lives within new limits. Pacing strategies — carefully planning activities to avoid overexertion — can help manage energy levels. Emotional support from family, friends, and support groups can make a tremendous difference. Flexible work arrangements, like remote work or part-time schedules, can enable some to maintain a career.
Moreover, finding new hobbies or passions that align with one's energy levels, such as writing, painting, or gardening, can bring immense satisfaction. Life with CFS may not be "normal" in the traditional sense, but it can still be meaningful, purposeful, and joyful.
Can You Push Through Chronic Fatigue?
The idea of "pushing through" is common advice for many life challenges, but when it comes to chronic fatigue, it can be harmful. Unlike ordinary tiredness or even temporary illness, CFS does not respond positively to forced exertion. In fact, pushing through symptoms often leads to post-exertional malaise (PEM), a hallmark of the condition where physical or mental exertion triggers a severe worsening of symptoms.
PEM can be devastating, reducing functionality for days, weeks, or even longer. It can feel like having the flu, compounded by a crash in cognitive abilities, emotional stability, and physical strength. Thus, pacing and energy management are vital. Patients are encouraged to respect their physical limitations and recognize the signs that they are approaching their limits. Rest, strategic planning, and sometimes saying "no" are essential self-care practices, not signs of weakness.
Healthcare providers often emphasize a "stop-rest-pace" approach: stopping activity before exhaustion hits, resting thoroughly, and pacing activities to maintain a sustainable level of energy. This approach stands in stark contrast to the "push through" mentality and can significantly enhance quality of life.
The Role of Waklert in the Management of the Condition
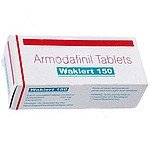
Managing CFS often requires a multi-faceted approach, combining lifestyle adjustments, psychological support, and sometimes medications to manage symptoms. One medication that has attracted interest is Waklert (Armodafinil), a wakefulness-promoting agent typically prescribed for conditions like narcolepsy and sleep apnea.
Waklert works by influencing neurotransmitters in the brain to enhance alertness and reduce feelings of extreme sleepiness. In some cases, it has been prescribed off-label to patients with chronic fatigue to help improve wakefulness, concentration, and overall energy levels.
However, the use of Waklert in CFS is nuanced. Not all patients respond positively, and some may experience side effects such as headaches, anxiety, nausea, or increased heart rate. It is not a cure for CFS but can be a tool to help manage specific symptoms, particularly when fatigue severely impairs daily functioning.
It is crucial that the decision to use Waklert be made under the close supervision of a healthcare professional. Physicians typically start with a low dose and monitor for efficacy and side effects. Additionally, Waklert should be part of a broader management strategy, including pacing, nutritional support, mental health care, and addressing sleep disturbances.
Waklert can offer a meaningful improvement for some, helping them regain a degree of functionality that otherwise might be unattainable. Nonetheless, expectations must be realistic; it is a supportive tool, not a standalone solution.
Final Thoughts
Chronic fatigue is a complex, life-altering condition that demands understanding, compassion, and a thoughtful approach to management. It feels like an overwhelming exhaustion that sleep cannot fix, not a character flaw or a failure of willpower. Distinguishing true fatigue from "laziness" is crucial for validating the experiences of those who suffer from CFS.
While living a "normal" life with CFS may not always be possible in the conventional sense, many find ways to adapt and create lives that are fulfilling and meaningful. The notion of pushing through fatigue can be dangerous, often resulting in more severe setbacks, so energy conservation strategies are vital.
Medications like Waklert may offer symptomatic relief for some patients, improving wakefulness and cognitive function. Yet, they are most effective when used as part of a holistic care plan designed to respect the unique challenges of chronic fatigue.
Ultimately, understanding CFS and supporting those affected by it requires a shift in societal attitudes — from viewing fatigue as a sign of weakness to recognizing it as a legitimate and serious medical condition deserving empathy, research, and better treatments.
Medically Reviewed by Dr. Mevan Nandaka Wijetunga, MD
(Updated at May 7 / 2025)