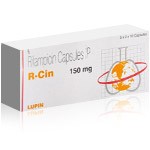
R-Cin Rifampicin Antibiotic for Tuberculosis and Bacterial Infections

R-Cin 90 (Rifampicin) is a well-established broad-spectrum antibiotic widely used in the treatment of serious bacterial infections, particularly those requiring long-term and targeted antimicrobial therapy. Rifampicin works by inhibiting bacterial RNA synthesis, which effectively stops the growth and multiplication of susceptible microorganisms.
This medication plays a critical role in the management of tuberculosis, leprosy, and certain severe staphylococcal infections, and is often used as part of combination antibiotic regimens to reduce the risk of bacterial resistance. R-Cin 90 is also utilized in specific cases of meningococcal prophylaxis and other infections where deep tissue penetration is required.
Due to its strong enzyme-inducing properties, Rifampicin requires careful monitoring and adherence to prescribed dosing schedules. When used correctly under medical guidance, R-Cin 90 provides reliable antibacterial activity and supports successful long-term infection control in complex clinical situations.
- Leprosy (Hansen’s Disease) – Part of multidrug therapy to eliminate Mycobacterium leprae;
- Meningococcal Prophylaxis – Prevents the spread of Neisseria meningitidis in individuals exposed to meningitis;
- Brucellosis – Combined with other antibiotics to treat bacterial infections from Brucella ;
- Legionnaires Disease – Used in severe cases caused by Legionella pneumophila;
- Endocarditis – Helps treat bacterial infections of the heart lining, especially caused by Staphylococcus aureus;
- Staphylococcal Infections – Used when resistance to other antibiotics is present.
- Broad Spectrum Antibiotic – Active against various Gram-positive and Gram-negative bacteria, making it useful for multiple infections;
- Prevents Drug Resistance in TB Treatment – Used in combination therapy to reduce the risk of antibiotic resistance;
- Rapid Bacterial Clearance – Inhibits bacterial RNA synthesis, effectively stopping bacterial replication and accelerating recovery;
- Essential for Leprosy Treatment – A key component in multidrug therapy for eliminating Mycobacterium leprae;
- Prophylaxis Against Meningitis – Prevents the spread of Neisseria meningitidis in close-contact individuals;
- Treats Serious Bacterial Infections – Used in cases of brucellosis, Legionnaires’ disease, and endocarditis, especially when other antibiotics fail;
- Penetrates Tissues Effectively – Reaches deep into tissues and infected cells, ensuring complete eradication of bacteria;
- Well-Tolerated in Most Patients – When used under medical supervision, it provides safe and effective bacterial control;
- Improves Treatment Outcomes – Enhances the success rate of long-term bacterial infection management, reducing recurrence risks.
Generic R-Cin (Rifampicin 150 mg) Medication guide:
💊 Drug Overview: R-Cin and Rifampicin Explained
R-Cin is a brand-name antibiotic that contains rifampicin (also spelled rifampin in some countries). This drug is best known for its role in treating tuberculosis (TB), but it is also used in other serious bacterial infections where a strong, targeted antibiotic approach is required. Rifampicin is not a “simple” everyday antibiotic - it has unique benefits, strict combination-therapy rules for certain infections, and a high interaction potential with many medications.
In clinical practice, rifampicin is valued because it can penetrate tissues well and is effective against specific bacteria, including mycobacteria. At the same time, it can strongly accelerate the breakdown of other drugs in the body (enzyme induction), which is why correct guidance and monitoring matter.
| Item | Summary |
|---|---|
| Brand and active ingredient | R-Cin (rifampicin); |
| Primary clinical role | Core medicine in multi-drug TB therapy and selected severe infections; |
| Key characteristic | Strong effect on drug metabolism (high interaction risk) and need for careful regimen planning; |
| Typical clinical approach | Often used as part of combination therapy rather than as a standalone antibiotic. |
What makes rifampicin different is not only what it treats, but also how it behaves in the body. Patients may notice a harmless discoloration of certain body fluids, while clinicians focus on liver safety and interaction control. Because the medicine can quickly select for resistant organisms if used incorrectly, it is especially important to follow the prescribed plan and not stop early.
Key takeaways for patients and caregivers:
- It is commonly used for serious infections that require structured therapy, not casual self-treatment;
- It may interact with many prescriptions and supplements, so medication disclosure is essential;
- Stopping early or using it incorrectly can increase resistance risk;
- Monitoring may be needed, especially for liver-related safety concerns.
This overview sets the foundation for the next sections, where we will define the brand vs generic difference, explain how the active ingredient works, and then move into official indications, dosing logic, safety, and clinically important interactions.
🏷️ Brand Name vs Generic Name: Understanding R-Cin (Rifampicin)
In pharmaceutical practice, distinguishing between a brand-name product and its generic counterpart is essential for correct prescribing, substitution, and patient understanding. R-Cin represents a branded formulation, while rifampicin is the internationally recognized active substance responsible for the drug’s antibacterial effect.
Regulatory authorities evaluate generic rifampicin products to ensure bioequivalence with branded versions. This means that although the brand name, tablet appearance, or capsule shell may differ, the medicine is required to deliver comparable blood concentrations and therapeutic outcomes when taken as directed.
Why brand names still matter clinically:
- They allow doctors to reference a specific manufacturer with known quality standards;
- They help pharmacies maintain consistency when supplying long-term therapy;
- They may differ in excipients, which can affect tolerability in sensitive patients;
- They simplify patient recognition during prolonged treatment courses.
A notable point with rifampicin is international naming. In many countries, including Europe and Asia, the name rifampicin is used, while in the United States the same molecule is commonly called rifampin. This difference is purely linguistic and regulatory; the chemical structure and antibacterial activity remain identical.
Clinical insight: For infections such as tuberculosis, treatment guidelines focus on the active molecule rather than the brand. However, switching between different brands mid-therapy without medical supervision is generally discouraged, as consistent formulation use supports stable blood levels and reduces adherence errors.
| Aspect | R-Cin (Brand) | Rifampicin (Generic) |
|---|---|---|
| Name purpose | Commercial product identifier; | Scientific and regulatory identifier; |
| Manufacturer | Specific pharmaceutical company; | Multiple licensed manufacturers worldwide; |
| Clinical effect | Driven by rifampicin content; | Identical antibacterial action; |
| Substitution rules | May be replaced with generic equivalents; | Requires quality and bioequivalence approval. |
Doctor’s perspective: “When prescribing rifampicin, I focus on the reliability of the formulation and patient adherence rather than the brand name alone. A trusted brand like R-Cin can help maintain consistency during long treatment cycles.”
Understanding this distinction prepares patients for the next step - learning about the pharmacological properties of rifampicin itself, which ultimately define its therapeutic role regardless of branding.
🧪 Active Ingredient Profile: Rifampicin Pharmacological Properties
The therapeutic effect of R-Cin is entirely driven by its active ingredient, rifampicin, a semi-synthetic antibiotic belonging to the rifamycin group. This compound is specifically designed to target bacteria at the genetic level, making it highly effective against certain hard-to-treat pathogens.
Rifampicin works by binding to bacterial DNA-dependent RNA polymerase. Once attached, it blocks RNA synthesis, preventing bacteria from producing essential proteins. Without these proteins, bacterial cells cannot survive or replicate. This mechanism is highly selective for bacterial enzymes and does not directly inhibit human RNA polymerase at therapeutic doses.
Key pharmacological feature: Rifampicin is bactericidal, meaning it kills bacteria rather than merely slowing their growth. This property is critical in infections where rapid bacterial elimination is required, such as tuberculosis and invasive staphylococcal infections.
From a chemical standpoint, rifampicin is a lipophilic molecule. This allows it to penetrate tissues, cells, and intracellular compartments efficiently. As a result, it can reach bacteria that are hidden inside cells, a characteristic that sets it apart from many standard antibiotics.
🩺 Clinical note: Because rifampicin strongly induces hepatic enzymes (especially CYP450 isoenzymes), it accelerates the metabolism of many drugs. This property is pharmacological rather than toxic, but it has major implications for treatment planning and drug selection.
| Property | Clinical Relevance |
|---|---|
| Bactericidal action | Rapid killing of susceptible bacteria; |
| Intracellular penetration | Effective against bacteria residing inside host cells; |
| Enzyme induction | Reduces blood levels of many co-administered drugs; |
| Lipophilicity | Wide tissue distribution including lungs and liver. |
👨⚕️ Expert insight: “Rifampicin is not interchangeable with routine antibiotics. Its pharmacological strength lies in deep tissue penetration and rapid bactericidal action, but this same power demands careful oversight due to its interaction profile.”
Understanding the pharmacological nature of rifampicin is essential before discussing its classification, approved uses, and dosing strategies. The next section will place this active ingredient within its formal drug class and therapeutic category.
🧬 Drug Class and Therapeutic Category
Rifampicin belongs to the rifamycin class of antibiotics, a distinct and highly specialized group developed for infections that require deep penetration, prolonged exposure, and strict therapeutic discipline. This classification immediately separates it from common outpatient antibiotics that are prescribed for short-term, uncomplicated infections.
From a therapeutic standpoint, rifampicin is categorized as a systemic antibacterial agent. This means its activity is not limited to a single tissue or surface environment. Instead, it distributes widely throughout the body, reaching organs, intracellular compartments, and sites where bacteria may remain dormant or protected from immune clearance.
Key Insight: The drug class of rifampicin explains why it is commonly reserved for protocol-driven therapies rather than empirical or trial-and-error treatment.
Clinically, rifampicin is most often positioned as a cornerstone drug within combination regimens. Its classification reflects not only antibacterial potency, but also its ability to prevent bacterial persistence and relapse when used correctly alongside companion antibiotics. This is especially important in infections where monotherapy would rapidly lead to resistance.
| Classification Level | Description | Clinical Meaning |
|---|---|---|
| Pharmacological class | Rifamycin antibiotic; | Targets bacterial RNA synthesis with bactericidal action; |
| Therapeutic category | Systemic antibacterial agent; | Acts throughout the body, not limited to one organ; |
| Primary clinical domain | Mycobacterial and selected severe bacterial infections; | Used when standard antibiotics are insufficient; |
| Typical regimen role | Combination-therapy core drug; | Prevents resistance and supports long-term eradication. |
Another defining feature of this drug class is its strong effect on hepatic enzyme systems. Rifampicin is a potent enzyme inducer, meaning it accelerates the metabolism of many other medications. This property is not incidental - it is directly linked to its pharmacological category and must be considered part of its therapeutic identity.
🧠 Why this classification matters in real practice
- It signals that treatment must follow established clinical protocols;
- It explains why rifampicin is rarely prescribed as monotherapy;
- It highlights the need to review all concurrent medications;
- It reinforces the importance of strict adherence and duration control.
Doctor’s perspective: When rifampicin appears in a treatment plan, it changes the entire therapeutic framework. The drug class alone tells the clinician that the infection is complex, the margin for error is small, and every supporting medication must be chosen deliberately.
Understanding the drug class and therapeutic category of rifampicin provides essential context for everything that follows - from its mechanism of action to its official indications, dosing strategies, and safety monitoring requirements.
⚙️ Mechanism of Action: How Rifampicin Works in the Body
Rifampicin acts at one of the most fundamental levels of bacterial survival - genetic transcription. Unlike antibiotics that damage cell walls or interfere with protein assembly later in the process, this drug stops bacteria at the moment they attempt to read and execute their genetic code.
At the molecular level, rifampicin binds directly to the bacterial DNA-dependent RNA polymerase enzyme. Once bound, it blocks the initiation of RNA synthesis. Without RNA, bacteria cannot produce essential proteins, enzymes, or structural components, leading to rapid bacterial death.
Key Concept: Rifampicin is bactericidal, not bacteriostatic. It does not slow bacterial growth - it actively eliminates susceptible organisms by shutting down transcription at its source.
A critical advantage of this mechanism is selectivity. Rifampicin has a high affinity for bacterial RNA polymerase and a very low affinity for the human equivalent. This selective binding allows effective bacterial killing at therapeutic doses without directly suppressing human cellular transcription.
| Target | Action of Rifampicin | Clinical Outcome |
|---|---|---|
| Bacterial RNA polymerase | Blocks initiation of RNA synthesis; | Rapid cessation of bacterial protein production; |
| Bacterial gene transcription | Prevents gene expression; | Loss of essential metabolic functions; |
| Intracellular bacteria | Penetrates host cells effectively; | Elimination of bacteria hidden inside cells. |
This mechanism is especially effective against slow-growing and intracellular organisms, such as mycobacteria. These pathogens are often resistant to antibiotics that act only on dividing cells, but rifampicin remains effective because transcription is required regardless of growth speed.
🧬 Why resistance develops quickly if misused
A single mutation in the RNA polymerase binding site can make bacteria resistant to rifampicin. This is why monotherapy is dangerous and why combination regimens are a non-negotiable rule for most indications.
Clinical insight: Rifampicin’s mechanism makes it one of the most powerful antibiotics in modern medicine - but also one of the least forgiving. Precision in dosing, duration, and combination choice directly determines whether the drug cures infection or accelerates resistance.
With the molecular mechanism established, the next section explores the spectrum of antibacterial activity and explains which pathogens are most susceptible to rifampicin-based therapy.
🧫 Spectrum of Antibacterial Activity
Rifampicin demonstrates a selective but highly strategic antibacterial spectrum. It is not designed to cover every common pathogen. Instead, its strength lies in targeting organisms that are persistent, slow-growing, intracellular, or prone to relapse when treated with standard antibiotics.
This spectrum explains why rifampicin is rarely chosen empirically. It is introduced deliberately, once the biological behavior of the pathogen is understood and a structured regimen is planned.
Clinical Insight: Rifampicin is most valuable when bacteria survive in protected niches - inside macrophages, within biofilms, or in tissues with limited antibiotic penetration.
The drug shows strong activity against mycobacteria, including Mycobacterium tuberculosis, which is the cornerstone of its global medical importance. In addition, rifampicin is active against selected gram-positive organisms, particularly when they form biofilms on prosthetic materials or damaged tissues.
| Pathogen Group | Activity Level | Clinical Relevance |
|---|---|---|
| Mycobacterium tuberculosis | Very high; | Backbone of standard TB treatment regimens; |
| Atypical mycobacteria | Moderate to high; | Used in selected non-tuberculous infections; |
| Staphylococcus aureus | High (in combination); | Effective against biofilm-associated infections; |
| Gram-negative bacteria | Limited; | Not used as a primary agent. |
Rifampicin’s ability to penetrate biofilms makes it particularly useful in infections involving prosthetic joints, heart valves, or indwelling medical devices. However, this same strength requires pairing with other antibiotics to avoid rapid resistance development.
🧠 Why spectrum matters more than breadth
A narrower spectrum reduces unnecessary disruption of normal microbiota while focusing lethal pressure on high-risk pathogens that demand aggressive control.
👨⚕️ Doctor’s remark: “When I use rifampicin, it is because the pathogen’s behavior calls for it - not because I want broader coverage. Precision is the real power of this drug.”
Understanding the antibacterial spectrum of rifampicin clarifies why it is reserved for specific scenarios and why treatment success depends on correct pathogen identification. The next section addresses official FDA-approved indications and how this spectrum translates into regulatory approval.
✅ FDA Approved Indications for Rifampicin
Rifampicin is a medically important antibiotic with official FDA-approved uses that are intentionally specific. This drug is not approved as a general “catch-all” antibacterial. Instead, the FDA indications focus on situations where rifampicin provides clear, high-value benefits and where structured treatment protocols reduce the risk of resistance.
In practice, the phrase FDA approved indications means the drug has been evaluated for safety and efficacy for a defined clinical purpose, under defined conditions. For rifampicin, those conditions typically involve protocol-based therapy, careful selection of patients, and often combination regimens rather than monotherapy.
🧾 FDA-approved uses commonly associated with rifampicin
- Tuberculosis (TB): Treatment of active tuberculosis as part of a multi-drug regimen;
- Latent TB infection: In specific guideline-driven protocols depending on clinical scenario;
- Meningococcal carriage: Elimination of Neisseria meningitidis from the nasopharynx in asymptomatic carriers to reduce transmission risk;
- Haemophilus influenzae type b (Hib) prophylaxis: Prevention of disease in close contacts in defined exposure situations.
The FDA indications for rifampicin include both treatment and prevention roles. This is unusual compared with many antibiotics, which are approved primarily for treatment. Rifampicin has specific approvals for reducing bacterial carriage in certain public health contexts, where stopping spread is the goal rather than curing an active infection.
The TB indication is the most recognized. For active tuberculosis, rifampicin is used because it is highly effective against mycobacteria and helps prevent relapse when used correctly. However, the FDA-approved approach emphasizes that rifampicin should be used with other anti-TB agents, since monotherapy can select resistant bacteria quickly.
Clinical Insight: For the FDA-approved infection-prevention indications (like meningococcal carriage), the goal is not to treat symptoms, but to interrupt transmission. That is why the dosing logic and duration differ from treatment regimens.
Another FDA-approved use is eradication of meningococcal carriage. A person may carry Neisseria meningitidis in the throat without illness, yet still transmit it to others. In such cases, rifampicin can be used to clear colonization and reduce outbreak risk, especially in household or close-contact exposure scenarios.
Rifampicin is also associated with prophylaxis in certain Haemophilus influenzae type b exposure contexts. This is not routine, and it is typically tied to specific risk settings, patient age groups, and public health guidance. The underlying concept is the same: rifampicin can eliminate the bacteria from the nasopharynx and reduce further spread.
| FDA Indication Type | Clinical Goal | Why Rifampicin Fits |
|---|---|---|
| Active TB treatment | Cure infection and prevent relapse; | High anti-mycobacterial potency and deep tissue penetration; |
| Carriage eradication (meningococcus) | Stop transmission in close-contact settings; | Effective at clearing nasopharyngeal colonization; |
| Contact prophylaxis (Hib) | Reduce secondary cases after exposure; | Prevents spread by eliminating colonization. |
👨⚕️ Doctor’s remark: “The FDA indications remind us that rifampicin is an antibiotic with public health impact. It is not only about curing - it can also be about controlling transmission, but only when used under the right rules.”
It is equally important to understand what FDA approval does not mean. It does not mean rifampicin is appropriate for routine respiratory infections, mild skin infections, or self-directed short courses. The drug’s approved profile reflects a balance: powerful benefit in specific indications, but a serious risk of resistance and interactions if used casually.
With FDA-approved indications clarified, the next section expands to off-label and internationally recognized uses, explaining where rifampicin is commonly used in real-world practice beyond the FDA label and why those uses exist.
🌍 Off-Label and Internationally Recognized Uses
Beyond its FDA-approved indications, rifampicin is widely used around the world in off-label and internationally recognized applications. These uses are grounded in strong clinical experience, regional guidelines, and real-world outcomes, even when they are not formally listed on the U.S. label. In many cases, global practice has moved faster than regulatory updates.
Off-label use does not mean experimental or unsafe. It means that physicians apply established pharmacology and evidence to clinical situations where rifampicin’s penetration, bactericidal action, and biofilm activity offer clear advantages over alternatives.
🌐 Global reality
In many countries, rifampicin is considered a core infectious disease tool, with indications defined by national TB programs, hospital protocols, and WHO-aligned recommendations rather than FDA labeling alone.
One of the most important off-label domains is the treatment of biofilm-associated infections. Rifampicin has the ability to penetrate bacterial biofilms, which are protective structures formed on artificial surfaces and damaged tissues. This makes it especially valuable in infections involving implants and prosthetic materials.
Another widely accepted international use is in complex staphylococcal infections, particularly when bacteria adhere to foreign bodies. In such cases, rifampicin is almost always used in combination with another antibiotic to reduce resistance risk while exploiting its deep penetration.
| Use Category | Typical Clinical Scenario | Why Rifampicin Is Chosen |
|---|---|---|
| Prosthetic joint infections | Infected hip or knee implants; | Biofilm penetration and intracellular activity; |
| Endocarditis (selected cases) | Valve-associated bacterial infection; | Enhanced bacterial eradication when combined; |
| Brucellosis | Systemic zoonotic infection; | High tissue penetration and synergy with other agents; |
| Leprosy (Hansen disease) | WHO-recommended multidrug therapy; | Rapid bactericidal effect against mycobacteria. |
Rifampicin is also used internationally for leprosy treatment as part of standardized multidrug therapy programs supported by the World Health Organization. In this context, its use is not considered experimental at all, but rather a global standard of care.
Another notable area is brucellosis, a zoonotic infection that can become chronic and difficult to eradicate. Rifampicin is often combined with other antibiotics to reduce relapse rates and improve long-term outcomes, especially in endemic regions.
Clinical Insight: Off-label rifampicin use is usually driven by pathogen behavior, not by infection location. If bacteria hide, persist, or form biofilms, rifampicin often becomes part of the discussion.
It is important to understand that off-label use does not remove the need for caution. In fact, it often increases responsibility. Dosing accuracy, combination choice, liver monitoring, and interaction management become even more critical outside of standardized FDA protocols.
⚠️ Important boundary
Off-label does not mean “free use.” Rifampicin should never be added casually to a regimen. Each off-label application requires a clear rationale, companion drugs, and a defined treatment duration.
Doctor’s perspective: Many infectious disease specialists view rifampicin as a “precision amplifier.” When used correctly, it strengthens a regimen dramatically. When used without structure, it can undermine future treatment options.
With international and off-label applications clarified, the next section focuses on the role of rifampicin in tuberculosis treatment regimens, where this drug remains one of the most critical components in global medicine.
🫁 Role of Rifampicin in Tuberculosis Treatment Regimens
Rifampicin is not just another drug in tuberculosis therapy - it is widely regarded as the backbone of modern TB treatment. Its introduction transformed tuberculosis from a disease requiring very long, relapse-prone therapies into one that could be treated with defined, time-limited regimens when used correctly.
In TB management, rifampicin is valued for two critical reasons: its powerful bactericidal effect against Mycobacterium tuberculosis and its ability to eliminate slow-growing and dormant bacterial populations. These bacterial subpopulations are responsible for prolonged infectivity and late relapse if not adequately suppressed.
🧩 Why rifampicin changed TB medicine
Before rifampicin-based regimens, TB treatment often extended beyond one year. Rifampicin made it possible to shorten therapy while maintaining cure rates, provided it is used consistently and in combination.
Standard TB regimens never rely on rifampicin alone. Instead, it is combined with other anti-tubercular agents to achieve multi-level bacterial suppression. Each drug in the regimen targets a different bacterial vulnerability, reducing the risk that resistant strains will emerge.
| Regimen Phase | Role of Rifampicin | Clinical Purpose |
|---|---|---|
| Intensive phase | Rapid bactericidal activity; | Reduce bacterial load and infectiousness; |
| Continuation phase | Sterilizing activity; | Eliminate persistent organisms and prevent relapse; |
| Long-term outcome | Resistance prevention; | Maintain durable cure when combined correctly. |
Another essential role of rifampicin in TB therapy is its impact on transmission control. By rapidly lowering bacterial counts in the lungs, the drug reduces how contagious a patient is early in treatment. This effect has major public health implications, particularly in high-burden regions.
However, this central role comes with strict rules. Rifampicin misuse in TB - such as missed doses, premature discontinuation, or unplanned monotherapy - is one of the leading drivers of rifampicin-resistant and multidrug-resistant TB. Once resistance develops, treatment becomes significantly longer, more toxic, and less predictable.
⚠️ Critical warning: In tuberculosis, rifampicin resistance is not a minor setback. It fundamentally changes the disease category and limits future treatment options.
From a clinical management perspective, rifampicin also influences treatment monitoring. Because it interacts with many drugs and affects liver enzymes, TB regimens are designed with these interactions in mind, especially in patients receiving antiretroviral therapy or other long-term medications.
👨⚕️ Doctor’s note: “In TB care, rifampicin is the anchor. If it is removed or compromised, the entire regimen weakens. That is why adherence and supervision matter as much as the drug itself.”
Understanding the role of rifampicin in tuberculosis regimens clarifies why this drug is protected, monitored, and carefully regulated worldwide. The next section examines how rifampicin functions within combination antibiotic therapy beyond tuberculosis, and why synergy matters just as much as potency.
🔗 Use of Rifampicin in Combination Antibiotic Therapy
Rifampicin is rarely prescribed as a standalone antibiotic. Its true clinical strength emerges when it is used as part of combination antibiotic therapy, where each drug plays a distinct and complementary role. This approach is not optional or stylistic - it is a core principle tied directly to rifampicin’s pharmacology.
The primary reason for combination use is resistance prevention. Rifampicin acts on a single, highly specific bacterial target. A single genetic mutation can confer resistance, which means that monotherapy creates strong selective pressure. Pairing rifampicin with other antibiotics dramatically reduces this risk by attacking bacteria through multiple independent mechanisms.
🧠 Core concept of combination therapy
Rifampicin is best understood as a potency amplifier. On its own, it is vulnerable to resistance. In combination, it enhances bacterial killing and improves long-term outcomes.
In clinical practice, rifampicin is often combined with agents that cover extracellular bacteria while rifampicin targets intracellular and biofilm-associated organisms. This dual approach ensures that bacteria cannot escape by shifting location or metabolic state.
| Clinical Scenario | Combination Rationale | Therapeutic Benefit |
|---|---|---|
| Tuberculosis | Multi-drug suppression; | Shorter therapy and lower relapse risk; |
| Prosthetic infections | Biofilm disruption + companion antibiotic; | Improved eradication of device-associated bacteria; |
| Chronic staphylococcal infections | Synergy with anti-staphylococcal agents; | Reduced persistence and recurrence. |
Another benefit of combination therapy is functional coverage. While rifampicin penetrates deeply into tissues and cells, partner antibiotics often provide broader extracellular coverage. This layered strategy reduces the likelihood of bacterial survival in mixed populations.
Clinical Insight: When rifampicin is added to a regimen, the entire drug interaction profile must be reassessed. It may lower blood levels of companion drugs, requiring dose adjustments or alternative selections.
Combination therapy also influences treatment duration. Rifampicin’s bactericidal activity allows regimens to be shorter and more decisive, provided adherence is strict. Missed doses or inconsistent intake undermine this advantage and can negate the benefits of combination design.
⚠️ Important reminder: Rifampicin should never be added or removed from a combination regimen without medical oversight. Doing so can destabilize the entire treatment strategy.
Doctor’s perspective: In combination therapy, rifampicin acts as a force multiplier. It raises the ceiling of what a regimen can achieve, but it also raises the stakes. Precision, planning, and monitoring are non-negotiable.
With combination therapy principles established, the next section examines indications by infection type and clinical scenario, translating theory into practical decision-making.
🧭 Indications by Infection Type and Clinical Scenario
Rifampicin is prescribed based on how an infection behaves, not simply where it is located. Its indications expand or narrow depending on whether bacteria are intracellular, slow-growing, biofilm-forming, or associated with foreign material. This section translates pharmacology into practical, scenario-based decision making.
Clinicians typically consider rifampicin when standard antibiotics struggle due to poor penetration, persistence, or high relapse risk. The decision is rarely binary; it involves weighing pathogen type, disease chronicity, device involvement, and the need for combination therapy.
🧩 How clinicians think about indications
The question is not “Can rifampicin work here?” but “Does this infection demand its unique strengths, and can we control its risks?”
In mycobacterial infections, rifampicin is indicated because these organisms replicate slowly and survive inside host cells. In staphylococcal infections, it is considered when bacteria form biofilms on prosthetic material, where conventional agents alone often fail. In public health scenarios, it is used to eliminate carriage and interrupt transmission rather than to treat symptoms.
| Infection Type | Typical Clinical Scenario | Why Rifampicin Is Considered |
|---|---|---|
| Mycobacterial disease | Active or latent tuberculosis; | High bactericidal activity against slow-growing organisms; |
| Biofilm-associated infections | Prosthetic joints, valves, hardware; | Penetrates biofilms and intracellular niches; |
| Chronic staphylococcal infection | Relapsing or device-related cases; | Synergy with companion antibiotics; |
| Carrier eradication | Meningococcal or Hib exposure; | Clears nasopharyngeal colonization. |
For acute, uncomplicated infections, rifampicin is generally not indicated. Its benefits do not outweigh the risks when bacteria are easily eradicated with simpler agents. This selective approach preserves rifampicin’s effectiveness for situations where it truly changes outcomes.
Clinical Insight: Indication strength increases when infections involve persistence, foreign material, or intracellular survival. It decreases when infections are superficial, rapidly responsive, or easily covered by first-line antibiotics.
Another key determinant is treatment context. In hospital settings, rifampicin may be used under close monitoring with tailored combinations. In outpatient or public health settings, its use is more restricted and protocol-driven to minimize misuse.
⚠️ Boundary reminder
An indication is not a green light for monotherapy. Most clinical scenarios that justify rifampicin also require companion drugs and a defined duration.
Doctor’s perspective: “When I match rifampicin to an indication, I’m matching it to a problem profile - persistence, protection, or transmission. If none of those are present, I usually look elsewhere.”
With indications mapped by infection type and scenario, the next section moves into dosage forms and available strengths, translating indication into practical prescribing options.
💊 Dosage Forms and Available Strengths
Rifampicin is manufactured in multiple dosage forms to support different treatment settings, patient populations, and clinical objectives. The choice of form is not cosmetic - it directly affects absorption consistency, adherence, and protocol compatibility, especially in long-term regimens such as tuberculosis therapy.
In routine practice, oral formulations dominate due to their reliability and convenience. Injectable forms are reserved for controlled environments where oral intake is not feasible or where rapid, supervised delivery is required. Pediatric-friendly options exist to ensure accurate dosing across age groups.
📦 Why multiple forms matter
Rifampicin regimens often last weeks or months. Having flexible dosage forms helps maintain adherence, reduce dosing errors, and align treatment with real-life patient needs.
The most commonly prescribed form is the oral capsule, which delivers predictable systemic exposure when taken correctly. Capsules are typically preferred for adults and adolescents, particularly in outpatient and continuation-phase therapy. Liquid formulations are often used in children or patients who have difficulty swallowing solid dosage forms.
Injectable rifampicin is generally limited to hospital settings. Its use is guided by strict protocols and is less common than oral therapy, reflecting rifampicin’s excellent oral bioavailability when administered properly.
| Dosage Form | Typical Strengths | Common Use Case |
|---|---|---|
| Oral capsules | 150 mg, 300 mg; | Standard adult and adolescent therapy; |
| Oral suspension | Concentration-based dosing; | Pediatric use or swallowing difficulty; |
| Injectable form | Hospital-prepared doses; | Controlled inpatient scenarios. |
Strength selection is typically guided by body weight, indication, and regimen structure. Rather than titrating small dose changes, clinicians often combine fixed-strength capsules to reach the required total daily dose. This approach simplifies prescribing and reduces dispensing errors.
Clinical Insight: Fixed strengths are intentional. They support standardized regimens and make it easier to detect missed doses, which is critical in infections where adherence determines cure.
It is also important to note that rifampicin is frequently included in fixed-dose combination products in some countries, especially for tuberculosis. These combinations are designed to improve adherence and reduce the risk of selective monotherapy, although availability varies by region.
Doctor’s perspective: Choosing the correct dosage form is part of treatment strategy. A formulation that fits the patient’s routine often matters as much as the milligram strength written on the prescription.
With dosage forms and strengths clarified, the next section moves into recommended dosage guidelines for adults, where form, strength, and clinical indication come together in practical dosing decisions.
📏 Recommended Dosage Guidelines for Adults
Adult dosing of rifampicin is guided by clinical indication, body weight, and regimen structure. Unlike many antibiotics where dosing can be loosely adjusted, rifampicin requires precision and consistency, because underdosing increases resistance risk while overdosing raises the likelihood of adverse effects, particularly hepatic stress.
In most adult treatment protocols, rifampicin is administered once daily. This is not for convenience alone. Once-daily dosing aligns with the drug’s pharmacokinetic profile and supports better adherence during long treatment courses, especially in tuberculosis and other chronic infections.
🧮 Dosing logic explained
Adult rifampicin doses are typically calculated based on body weight ranges, then rounded to available capsule strengths to ensure simplicity, accuracy, and regimen standardization.
For tuberculosis and most serious infections, rifampicin is taken on an empty stomach, usually 30 to 60 minutes before food. This timing improves absorption and helps maintain predictable blood concentrations, which is especially important when rifampicin is part of a multi-drug protocol.
| Adult Weight Range | Typical Daily Dose | Administration Pattern |
|---|---|---|
| Under 50 kg | 450 mg; | Once daily, usually morning; |
| 50 kg and above | 600 mg; | Once daily, on an empty stomach; |
| Selected non-TB indications | Protocol-dependent; | Defined duration and combination therapy. |
In non-tuberculosis indications, dosing may differ depending on the infection type, duration of therapy, and companion antibiotics. These regimens are usually shorter but still require strict adherence to avoid partial bacterial suppression.
Clinical Insight: Skipping doses or taking rifampicin at inconsistent times can reduce effective drug exposure even if the total milligram dose appears correct.
Dose adjustments may be considered in patients with hepatic impairment, concurrent hepatotoxic medications, or complex drug interaction profiles. In these cases, dosing decisions are individualized and often paired with laboratory monitoring rather than simple milligram changes.
👨⚕️ Doctor’s perspective: “With rifampicin, the right dose taken the right way matters more than small milligram adjustments. Consistency is what protects both the patient and the future effectiveness of the drug.”
Understanding adult dosage guidelines is essential before addressing special populations. The next section focuses on pediatric dosage considerations, where weight-based precision becomes even more critical.
👶 Pediatric Dosage Considerations
Dosing rifampicin in pediatric patients requires a different clinical mindset than in adults. Children are not simply “small adults” - their metabolism, liver enzyme activity, and drug clearance rates vary significantly by age, growth stage, and overall health status. Because rifampicin strongly interacts with metabolic pathways, precision in pediatric dosing is especially important.
Pediatric regimens are almost always weight-based and are adjusted as the child grows. This dynamic dosing approach ensures adequate antibacterial exposure while minimizing toxicity risk. Regular reassessment is a core part of therapy, particularly during longer treatment courses such as tuberculosis management.
📐 How pediatric dosing is determined
Pediatric rifampicin doses are calculated per kilogram of body weight and then aligned with available formulations to maintain accuracy and adherence.
Oral liquid formulations are often preferred for infants and younger children because they allow for fine dose adjustments and easier administration. Older children and adolescents may transition to capsules once swallowing is reliable and dosing stabilizes.
| Age Group | Typical Dosing Approach | Clinical Focus |
|---|---|---|
| Infants and toddlers | Strict mg/kg dosing; | Close monitoring and formulation flexibility; |
| Children | Weight-adjusted daily dosing; | Growth-related dose reassessment; |
| Adolescents | Transition toward adult protocols; | Adherence and interaction awareness. |
Because rifampicin induces liver enzymes, pediatric patients receiving other long-term medications may require dose adjustments of companion drugs. This is particularly relevant in children with chronic conditions who rely on anticonvulsants or hormonal therapies.
Clinical Insight: In children, missed doses or incorrect measurement of liquid formulations can significantly alter effective exposure, even when parents believe therapy is being followed correctly.
Safety monitoring in pediatric use focuses on liver function, overall tolerance, and signs of hypersensitivity. While rifampicin is generally well tolerated in children when used correctly, vigilance remains essential due to treatment duration and interaction potential.
👨⚕️ Doctor’s perspective: “In pediatric rifampicin therapy, accuracy protects outcomes. Weight checks, formulation choice, and parental education are as important as the prescription itself.”
With pediatric dosing clarified, the next section addresses administration guidelines and best practices, focusing on how rifampicin should be taken to achieve optimal absorption and consistent therapeutic levels.
🕒 Administration Guidelines and Best Practices
Proper administration of rifampicin is as important as choosing the correct dose. Even when the prescription is accurate, how and when the medication is taken can significantly influence absorption, blood levels, and overall treatment success. This is especially true for long-term, protocol-based therapies.
Rifampicin is typically administered once daily, and consistency is critical. Taking the drug at the same time each day helps maintain stable plasma concentrations and supports adherence, which directly affects outcomes in infections such as tuberculosis.
⏰ Timing matters
Rifampicin is best taken on an empty stomach, usually 30 to 60 minutes before meals. Food can reduce absorption and lead to lower, less predictable drug levels.
Capsules should be swallowed whole with water. Crushing or opening capsules is generally discouraged unless a liquid formulation is specifically prescribed. For pediatric or special-care patients, liquid suspensions should be measured with a calibrated dosing device rather than household utensils.
Another important aspect of administration is coordination with other medications. Rifampicin can reduce the effectiveness of many drugs by accelerating their metabolism. To minimize interaction impact, clinicians often plan dosing schedules carefully or adjust companion medications.
| Best Practice | Reason | Clinical Benefit |
|---|---|---|
| Take at the same time daily | Maintains stable drug levels; | Improves efficacy and adherence; |
| Empty-stomach administration | Maximizes absorption; | Predictable therapeutic exposure; |
| Use proper measuring tools | Avoids dosing errors; | Accurate pediatric and liquid dosing. |
Patients should be informed that rifampicin can cause a harmless reddish-orange discoloration of urine, sweat, saliva, and tears. While this effect is expected, it can stain contact lenses and clothing, so advance awareness prevents unnecessary concern.
Clinical Insight: Inconsistent timing or taking rifampicin with food may not cause immediate symptoms, but it can silently reduce treatment effectiveness and increase resistance risk over time.
Adherence support is a key part of administration strategy. In some treatment programs, especially for tuberculosis, directly observed therapy (DOT) is used to ensure doses are taken correctly and consistently.
👨⚕️ Doctor’s perspective: “Most rifampicin failures are not about the drug - they are about timing, consistency, and interactions. Administration discipline protects the entire regimen.”
With administration best practices established, the next section explores food interactions and optimal timing strategies, explaining what to avoid and how to integrate rifampicin smoothly into daily routines.
🍽️ Food Interactions and Timing of Administration
Rifampicin is one of those antibiotics where timing is not a formality. The presence of food in the stomach can change how much of the drug actually reaches the bloodstream. This does not mean the medication stops working, but it can make its effect less predictable, which is undesirable in infections that depend on precise drug exposure.
When rifampicin is taken with food, absorption may be delayed or reduced. For short courses this might not always be clinically visible, but in long, structured regimens (especially tuberculosis therapy), small daily reductions can accumulate and affect outcomes.
Key rule in practice: Rifampicin is best taken on an empty stomach, ideally 30–60 minutes before meals, to achieve the most reliable blood levels.
That said, real life is not always ideal. Some patients experience mild stomach discomfort when taking rifampicin without food. In such cases, clinicians may allow administration with a small, non-fatty meal, accepting slightly reduced absorption in exchange for better adherence. This decision is individual and should not be self-adjusted.
Certain foods and drinks deserve special mention. High-fat meals tend to interfere more with absorption than light meals. Alcohol does not directly block rifampicin absorption, but it increases liver stress, which is already a consideration with this drug.
🧠 Clinical Insight
Timing consistency often matters more than perfection. Taking rifampicin the same way every day (same time, same relation to food) helps stabilize drug exposure, even if conditions are not ideal.
Another practical aspect is coordination with other medications. Because rifampicin affects drug metabolism, spacing doses does not always eliminate interactions, but predictable timing helps clinicians anticipate and manage them more effectively.
👨⚕️ Doctor’s perspective: “I don’t just ask if patients take rifampicin. I ask how they take it. Food timing explains many cases where the drug seems to ‘work less’ without obvious reason.”
Understanding food interactions and timing sets the stage for the next topic - how long rifampicin should be taken and why treatment duration and compliance are inseparable concepts in successful therapy.
⏳ Duration of Therapy and Treatment Compliance
With rifampicin, duration is not flexible in the casual sense. The length of therapy is chosen to match how long bacteria can survive under pressure, not how quickly symptoms disappear. Many patients feel better early, but rifampicin is specifically used to eliminate persistent bacterial populations that would otherwise cause relapse.
Treatment duration varies widely depending on the indication. In some preventive or carrier-eradication scenarios, therapy may last only a few days. In contrast, tuberculosis and other chronic infections require months of uninterrupted treatment. The common thread is that the endpoint is defined by microbiological logic, not comfort.
🧭 How clinicians define treatment length
Duration is chosen to outlast bacterial survival strategies. Rifampicin stays in the regimen long enough to prevent dormant organisms from reactivating once therapy stops.
Compliance is where rifampicin either delivers its full benefit or fails silently. Missing doses does not usually cause immediate worsening, which can give a false sense of safety. However, each missed dose creates a window where bacteria are exposed to sublethal pressure, increasing the risk of resistance development.
For this reason, many public health programs treat rifampicin compliance as a core therapeutic parameter, not a secondary concern. Tools such as treatment calendars, reminders, and supervised dosing exist precisely because adherence determines success.
⚠️ Critical point: Stopping rifampicin early or taking it inconsistently can convert a treatable infection into a resistant one, even if symptoms initially improve.
Another challenge is treatment fatigue. Long courses can erode motivation, especially when daily life returns to normal. This is why clinicians emphasize planning ahead - travel, work schedules, and routine disruptions should be anticipated rather than handled reactively.
In tuberculosis care, structured approaches such as directly observed therapy exist not because patients are distrusted, but because the consequences of non-compliance extend beyond the individual to the community.
👨⚕️ Doctor’s perspective: “Rifampicin doesn’t forgive shortcuts. When patients finish the full course exactly as planned, outcomes are excellent. When they don’t, the drug often gets blamed for a human problem.”
Understanding duration and compliance prepares the ground for the next section, which addresses what to do if a dose is missed and how to respond without compromising the entire regimen.
⏰ What Happens if a Dose Is Missed
Missing a dose of rifampicin is not a rare event, but the response to a missed dose is what determines whether the treatment remains effective. Unlike painkillers or short-course antibiotics, rifampicin works within a tightly balanced exposure window, especially in long-term regimens.
The impact of a missed dose depends on how often it happens, how long therapy has been ongoing, and which infection is being treated. One isolated mistake is usually manageable, but repeated misses can quietly undermine the entire regimen.
- If you remember within the same day: take the missed dose as soon as possible;
- If it is close to the next scheduled dose: skip the missed dose and continue as planned;
- Do not double the dose to compensate for a missed one;
- Return to your regular schedule immediately after.
Doubling doses does not restore lost effectiveness and can increase the risk of side effects, particularly liver-related reactions. Rifampicin relies on consistent daily pressure, not occasional high peaks.
⚠️ Important warning: Repeated missed doses increase the risk of rifampicin resistance, even if the total number of tablets taken seems high.
In long-term treatments such as tuberculosis, clinicians may adjust monitoring or provide additional adherence support if missed doses become frequent. The goal is not punishment, but protecting the effectiveness of the therapy.
- Recognize the missed dose without panic;
- Resume the correct schedule immediately;
- Inform your healthcare provider if misses occur more than once;
- Use reminders or pill organizers to prevent recurrence.
Missed doses during short prophylactic courses may require different actions than those during long TB regimens. This is why self-correction should be limited to isolated incidents, while patterns should always be discussed with a professional.
👨⚕️ Doctor’s perspective: “One missed dose can be managed. A pattern of missed doses changes the biology of the infection. That difference is where resistance is born.”
Understanding how to respond to missed doses leads naturally into the next topic - overdose symptoms and emergency measures, which addresses the opposite scenario and its risks.
🚨 Overdose Symptoms and Emergency Measures
Rifampicin overdose is uncommon, but when it occurs, it requires immediate attention. Unlike gradual side effects that build over time, overdose reactions tend to appear suddenly and can involve multiple organ systems, especially the liver and gastrointestinal tract.
Overdose most often happens due to accidental double dosing, confusion between capsule strengths, or combining rifampicin with other hepatotoxic substances. Intentional overdose is rare but medically serious.
Possible overdose symptoms may include:
- Severe nausea, vomiting, or abdominal pain;
- Intense fatigue, dizziness, or confusion;
- Marked yellowing of the skin or eyes (jaundice);
- Dark urine combined with pale stools;
- Rapid heartbeat or shortness of breath;
- Pronounced orange-red discoloration of body fluids beyond the usual level.
One characteristic but misleading sign is dramatic discoloration of urine, sweat, saliva, or tears. While mild discoloration is expected at normal doses, sudden intensification together with systemic symptoms may signal overdose or acute toxicity.
What to do immediately:
- Stop taking rifampicin until medical advice is received;
- Seek emergency medical care or contact poison control;
- Provide exact information about the dose taken and timing;
- Do not attempt self-treatment or induce vomiting.
There is no specific antidote for rifampicin overdose. Management focuses on supportive care, monitoring liver function, maintaining hydration, and treating symptoms. In hospital settings, clinicians may perform laboratory testing to assess hepatic stress and metabolic disturbances.
⚠️ Critical reminder: Do not compensate for missed doses by taking extra rifampicin. Overdose does not restore effectiveness and significantly increases toxicity risk.
Patients with pre-existing liver disease, alcohol use, or concurrent hepatotoxic medications are at higher risk of severe outcomes after overdose and should treat any dosing error as urgent.
👨⚕️ Doctor’s perspective: “With rifampicin, overdose is rarely dramatic at first glance, but the liver remembers everything. Early medical evaluation can prevent long-term damage.”
Knowing how to respond to overdose situations completes the picture of dose safety. The next section focuses on pharmacokinetics, explaining how rifampicin is absorbed, distributed, metabolized, and eliminated from the body.
🧪 Pharmacokinetics: Absorption, Distribution, Metabolism, Excretion
Pharmacokinetics explains what the body does to rifampicin after you swallow a capsule - how it gets absorbed, where it travels, how it is transformed, and how it leaves the body. With this drug, pharmacokinetics is not “background science”. It directly affects timing rules, interaction risk, and why rifampicin must be taken consistently.
A simple way to understand rifampicin pharmacokinetics is to treat it like a drug with two personalities: it is very effective systemically, but it also actively changes the body’s metabolism environment. This is why its PK profile is closely linked to clinical decision-making.
🧩 PK snapshot in one line
Rifampicin is well absorbed orally, widely distributed into tissues, metabolized in the liver, and eliminated mainly through bile and feces, with some urinary excretion.
Absorption: Rifampicin is absorbed from the gastrointestinal tract, and absorption is generally strong when taken correctly. Food can reduce or delay absorption, which is why protocols often recommend dosing on an empty stomach. What matters clinically is not only “how much” gets absorbed, but how predictable the absorption is day to day.
Distribution: After absorption, rifampicin spreads widely through the body, reaching many tissues and cellular compartments. This broad distribution is one reason rifampicin is valuable in infections where bacteria can hide in tissues or inside host cells. Its distribution profile supports its use in structured regimens where deep penetration is required.
- Wide tissue penetration supports treatment of persistent infections;
- Intracellular reach helps target bacteria sheltered from other antibiotics;
- Body-fluid discoloration is explained by distribution and excretion pathways.
Metabolism: Rifampicin is primarily processed by the liver. A key PK feature is that it can speed up metabolic enzyme activity over time. This means the body may begin clearing rifampicin (and many other drugs) faster after repeated dosing. Clinically, this contributes to the drug’s well-known interaction profile and why co-medications often need careful review.
Clinical Insight: Rifampicin can change the effective levels of many medications because it accelerates liver metabolism. PK here is not theory - it is the reason clinicians ask for a full medication list before and during therapy.
Excretion: Elimination occurs mainly through the biliary route into the gastrointestinal tract, which is why fecal excretion is significant. A portion is excreted in urine. The famous orange-red discoloration of urine, sweat, and tears is tied to rifampicin and its metabolites leaving the body - expected, usually harmless, but important for patients to anticipate.
👨⚕️ Doctor’s perspective: “Rifampicin pharmacokinetics is the hidden engine behind the whole regimen. If absorption is inconsistent or interactions are ignored, the plan looks correct on paper but fails in real life.”
With the full pharmacokinetic path covered (absorption to excretion), the next section focuses on impact on liver enzymes and drug metabolism, which is where rifampicin becomes uniquely challenging compared with most antibiotics.
🧬 Impact on Liver Enzymes and Drug Metabolism
One of the most defining characteristics of generic rifampicin is not how it kills bacteria, but how profoundly it changes the body’s internal chemistry. This medication is a powerful inducer of liver enzymes, and this single property influences almost every clinical decision around its use.
In practical terms, rifampicin accelerates the activity of hepatic enzyme systems, especially those involved in drug metabolism. When these enzymes become more active, the body begins to break down many medications faster than expected. As a result, blood levels of certain drugs may fall below their effective range even if doses remain unchanged.
This effect does not happen instantly. Enzyme induction develops gradually over several days of therapy and may persist for a period even after rifampicin is stopped. That delayed behavior is one reason interactions are sometimes overlooked or misunderstood.
🔬 Why enzyme induction matters
Rifampicin does not block other drugs. It makes the body eliminate them faster, silently reducing their effectiveness.
Medications commonly affected include hormonal therapies, anticoagulants, antiepileptic drugs, immunosuppressants, and many antivirals. In some cases, loss of effectiveness can be clinically significant, leading to treatment failure unrelated to the primary infection.
- Reduced levels of co-administered drugs without obvious symptoms;
- Need for dose adjustments or alternative medications;
- Risk persists even with correct rifampicin dosing;
- Interactions may continue briefly after discontinuation.
From a safety standpoint, the liver itself is usually resilient when rifampicin is used correctly. However, combining enzyme induction with other hepatotoxic agents or alcohol can increase liver strain, especially during prolonged therapy.
Clinical Insight: Many rifampicin “failures” are not bacterial resistance but metabolic interactions that quietly neutralize companion drugs.
This enzyme-inducing property is consistent across branded and generic formulations. Whether prescribed as R-Cin or another generic rifampicin product, the metabolic impact remains the same because it is driven by the active molecule itself.
👨⚕️ Doctor’s perspective: “Whenever I prescribe generic rifampicin, I review the entire medication list. Ignoring enzyme induction is one of the fastest ways to compromise an otherwise perfect treatment plan.”
Understanding how rifampicin reshapes drug metabolism prepares us for the next section, which focuses on common side effects and how to distinguish expected reactions from clinically significant problems.
⚠️ Possible Side Effects of Rifampicin and How to Manage Them
Generic rifampicin is a potent antibiotic that is generally well tolerated when used correctly, especially within structured regimens. However, due to its strong metabolic activity and long-term use in many indications, side effects may occur. Understanding them clearly helps patients stay compliant and recognize when action is needed.
Important context: Many side effects of rifampicin are related to enzyme induction, timing, or adaptation rather than toxicity. Most are reversible and manageable.
🟢 Common and Usually Mild Side Effects
- Gastrointestinal discomfort: nausea, mild abdominal pain, loose stools;
- Reduced appetite: especially during the first weeks of therapy;
- Fatigue or low energy: often transient and improves with routine;
- Headache: usually mild and self-limiting;
- Orange-red discoloration of body fluids: urine, sweat, saliva, tears.
These effects typically appear early and fade as the body adjusts. The discoloration effect is expected and harmless.
🟠 Visual effect explained: Rifampicin pigments are excreted through urine and tears. This may permanently stain soft contact lenses but does not indicate organ damage.
🟡 Moderate Side Effects (Require Monitoring)
- Elevated liver enzymes on blood tests;
- Persistent gastrointestinal upset;
- Mild skin itching or rash;
- Flu-like symptoms with intermittent dosing;
- Increased sensitivity to alcohol.
These effects do not always require stopping therapy but should be discussed with a healthcare provider if they persist or worsen.
🔴 Serious but Rare Adverse Reactions
| Side Effect | What It May Indicate | Action Required |
|---|---|---|
| Severe allergic reaction | Hypersensitivity or immune response; | Stop medication and seek emergency care; |
| Jaundice or dark urine | Possible liver injury; | Immediate medical evaluation; |
| Severe fatigue with confusion | Systemic reaction or hepatic stress; | Urgent consultation required. |
💡 How to Reduce Side Effects
- Take rifampicin consistently at the same time each day;
- Avoid alcohol during therapy;
- Stay well hydrated;
- Follow food timing instructions strictly;
- Inform your doctor about all other medications.
👨⚕️ Clinical Perspective: “With generic rifampicin, side effects often reflect metabolic adjustment rather than toxicity. Clear patient education prevents unnecessary discontinuation and protects treatment success.”
Recognizing and managing side effects effectively allows rifampicin therapy to remain both safe and highly effective. The next section focuses on serious drug interactions and why rifampicin requires special attention when combined with other medications.
🔄 Drug Interactions of Rifampicin - What You Must Know
Generic rifampicin is one of the most interaction-prone antibiotics in clinical practice. Its ability to strongly activate liver enzymes means it can reduce the effectiveness of many commonly used medications, sometimes without obvious warning signs. Understanding these interactions is essential for both safety and treatment success.
Unlike simple drug-drug conflicts, rifampicin interactions are metabolic. The medication accelerates drug breakdown rather than blocking absorption, which makes interactions less visible but more dangerous if overlooked.
🚨 High-Risk Drug Interactions (Critical)
- Oral contraceptives: significant loss of contraceptive effectiveness;
- Warfarin and anticoagulants: reduced anticoagulation, clot risk;
- Antiretroviral therapy (HIV): loss of viral suppression;
- Immunosuppressants (cyclosporine, tacrolimus): transplant rejection risk;
- Certain antifungals: reduced antifungal activity.
These interactions usually require therapy modification or alternative medications. Dose adjustment alone is often insufficient.
⚠️ Moderate Interactions (Monitoring Required)
- Antidiabetic drugs: reduced glucose control;
- Antiepileptic medications: seizure threshold changes;
- Corticosteroids: reduced anti-inflammatory effect;
- Beta blockers: reduced cardiovascular control;
- Thyroid hormones: altered hormone levels.
These interactions often require laboratory monitoring and possible dose recalibration during rifampicin therapy.
🍷 Lifestyle and Supplement Interactions
- Alcohol: increases liver strain and side-effect risk;
- Herbal supplements: unpredictable metabolism changes;
- Vitamin D and fat-soluble vitamins: altered blood levels;
- Protein supplements: generally safe, but timing consistency matters.
📊 Interaction Risk Overview
| Interaction Category | Clinical Risk | Recommended Action |
|---|---|---|
| Hormonal & anticoagulants | High; | Avoid or switch therapy; |
| Chronic disease medications | Moderate; | Monitor and adjust dose; |
| Supplements & alcohol | Variable; | Use caution and consistency. |
Clinical Insight: Rifampicin interactions often appear weeks after therapy starts. Stable patients may suddenly destabilize due to accelerated drug clearance.
👨⚕️ Expert Commentary: “Every time I prescribe generic rifampicin, I assume an interaction exists until proven otherwise. A full medication review is mandatory, not optional.”
Understanding rifampicin’s interaction profile is essential before initiating therapy. The next section addresses use in special populations, where interactions and safety considerations become even more critical.
👥 Use of Rifampicin in Special Populations
Prescribing generic rifampicin becomes more nuanced when patients fall into special population groups. Age, pregnancy status, organ function, and comorbid conditions can significantly alter both risk profile and management strategy. This section highlights how clinicians adapt therapy without compromising effectiveness.
🤰 Pregnancy
Rifampicin may be used during pregnancy only when the benefit outweighs potential risks. It has been widely used in tuberculosis protocols involving pregnant patients under close supervision.
- May reduce vitamin K levels in the mother;
- Vitamin K supplementation may be recommended near delivery;
- Requires coordinated obstetric and infectious disease oversight.
🤱 Breastfeeding
Rifampicin passes into breast milk in small amounts. In most cases, breastfeeding is not contraindicated, but infants should be monitored for gastrointestinal upset or unusual discoloration.
👴 Elderly Patients
Older adults often tolerate rifampicin well, but they are more likely to take multiple medications. This increases the risk of clinically significant drug interactions and warrants careful review of all concurrent therapies.
- Higher likelihood of polypharmacy;
- Increased sensitivity to liver enzyme induction;
- Closer monitoring recommended during long regimens.
🫀 Patients with Liver Disease
Because rifampicin is metabolized in the liver, pre-existing hepatic conditions increase the risk of enzyme elevation. Baseline and periodic liver function tests are essential.
🧪 Renal Impairment
Unlike many antibiotics, rifampicin does not rely heavily on renal clearance. Dose adjustment is usually not required solely due to kidney dysfunction, but overall tolerance should still be assessed.
🛡️ Immunocompromised Patients
Patients with weakened immune systems often benefit from rifampicin’s potent bactericidal activity, but they also face higher risks if interactions reduce companion drug effectiveness.
Coordination between specialties is critical to maintain therapeutic balance.
Clinical Insight: Special populations do not automatically exclude rifampicin use, but they require a more deliberate prescribing strategy with monitoring tailored to individual risk.
👨⚕️ Expert Commentary: “With generic rifampicin, special populations demand attention, not avoidance. Most complications arise from missed interactions, not from the drug itself.”
After addressing special populations, the next section focuses on laboratory monitoring and follow-up tests, which help ensure safety throughout rifampicin therapy.
🧪 Laboratory Monitoring and Follow-Up Tests
When treating with generic rifampicin, laboratory monitoring is not a formality - it is a safety net. Because this medication can influence liver enzymes, blood chemistry, and the effectiveness of other drugs, planned follow-up testing helps detect problems early, often before symptoms appear.
The intensity of monitoring depends on treatment duration, dose, and patient risk profile. Short courses may require minimal testing, while long-term regimens demand a structured approach.
📌 Baseline Tests (Before Starting Therapy)
- Liver function tests (ALT, AST, bilirubin): establish a reference point;
- Complete blood count (CBC): detect pre-existing abnormalities;
- Medication review: identify drugs affected by enzyme induction;
- Pregnancy status: when clinically relevant.
Baseline values are essential because mild laboratory changes during therapy may be acceptable if they remain close to starting levels. Without a baseline, interpretation becomes difficult and may lead to unnecessary treatment interruption.
🔁 Routine Monitoring During Treatment
During ongoing therapy, testing frequency is adjusted based on risk factors such as age, liver history, alcohol use, and polypharmacy.
- Liver enzymes at regular intervals;
- Clinical assessment for fatigue, nausea, jaundice;
- Review of newly added medications;
- Adherence confirmation and timing review.
📊 Typical Monitoring Overview
| Parameter | Why It Matters | Action if Abnormal |
|---|---|---|
| Liver enzymes | Detect hepatic stress; | Adjust dose or pause therapy; |
| Complete blood count | Monitor systemic effects; | Investigate if persistent changes; |
| Drug levels (selected cases) | Confirm therapeutic exposure; | Modify companion medication dosing. |
⚠️ When Results Require Immediate Attention
- Rapid enzyme elevation with symptoms;
- Marked bilirubin increase;
- Laboratory changes combined with clinical decline.
In many cases, mild laboratory abnormalities can be observed without stopping therapy. The key is trend interpretation, not isolated numbers.
👨⚕️ Clinical Perspective: “Most rifampicin-related lab changes are manageable. Problems arise when monitoring is skipped or results are ignored rather than interpreted in context.”
With monitoring principles in place, the next section focuses on long-term safety considerations and what is known about extended rifampicin use over time.
💊 Interaction with Oral Contraceptives and Hormonal Therapies
Generic rifampicin has a well-documented and clinically significant interaction with hormonal medications. This includes oral contraceptives, hormonal patches, implants, injections, and certain hormone replacement therapies. The interaction is not subtle and should be assumed to be present unless proven otherwise.
The mechanism is metabolic. Rifampicin strongly induces liver enzymes that accelerate the breakdown of hormones, leading to lower circulating hormone levels. As a result, medications that rely on stable hormone concentrations may become less effective or ineffective.
⚠️ Key warning: Rifampicin can significantly reduce contraceptive protection, increasing the risk of unintended pregnancy even when pills are taken correctly.
This interaction affects both estrogen-containing and progestin-only contraceptives. Switching brands or increasing pill strength does not reliably solve the problem, because enzyme induction continues to lower hormone exposure across formulations.
- Combined oral contraceptive pills;
- Progestin-only pills;
- Hormonal patches and vaginal rings;
- Hormonal implants and injections;
- Certain hormone replacement therapies.
In clinical practice, non-hormonal contraception methods are often recommended for the entire duration of rifampicin therapy and for a short period after discontinuation, as enzyme induction may persist temporarily.
| Hormonal Method | Effect of Rifampicin | Recommended Strategy |
|---|---|---|
| Oral contraceptive pills | Marked reduction in effectiveness; | Use non-hormonal backup; |
| Implants and injections | Reduced hormone levels; | Consult specialist for alternatives; |
| Hormone replacement therapy | Possible symptom recurrence; | Monitor and adjust therapy. |
For patients using hormonal therapy for non-contraceptive reasons, such as menstrual regulation or menopausal symptoms, rifampicin may lead to symptom breakthrough. This does not necessarily indicate disease progression but reflects reduced hormone exposure.
Clinical Insight: Enzyme induction begins within days and may persist after rifampicin is stopped. Contraceptive protection should not be resumed immediately without guidance.
👨⚕️ Doctor’s perspective: “With rifampicin, I assume hormonal therapy will underperform. Counseling and backup planning are essential parts of prescribing.”
Understanding hormonal interactions is especially important for patients of reproductive age. The next section addresses interaction with antiretroviral and antifungal drugs, where metabolic effects can also alter treatment outcomes.
🧬 Interaction with Antiretroviral and Antifungal Drugs
When generic rifampicin is combined with antiretroviral (ARV) or antifungal medications, interactions are often clinically decisive. These combinations can determine whether infections are controlled or whether therapy quietly fails due to reduced drug exposure.
The core issue is metabolic acceleration. Rifampicin induces hepatic enzymes that many ARVs and antifungals rely on for stable blood levels. The result is often a sharp drop in drug concentration, even when doses appear correct and adherence is perfect.
🧠 Antiretroviral Therapy (HIV)
Rifampicin can significantly reduce plasma levels of several antiretroviral agents, increasing the risk of viral breakthrough and resistance.
- Protease inhibitors: marked reduction, often contraindicated;
- Non-nucleoside reverse transcriptase inhibitors: variable reduction;
- Integrase inhibitors: may require dose adjustment or substitution.
In regions with high TB-HIV co-infection rates, clinicians often redesign ARV regimens specifically to accommodate rifampicin. This may include switching agents, adjusting doses, or choosing alternative TB drugs when feasible.
🍄 Antifungal Therapy
Many systemic antifungals depend on stable metabolism for efficacy. Rifampicin can render some of them subtherapeutic.
- Azoles (e.g., itraconazole, voriconazole): major reduction in levels;
- Fluconazole: moderate reduction, monitoring required;
- Amphotericin B: minimal metabolic interaction.
📊 Interaction Impact Overview
| Drug Group | Effect of Rifampicin | Clinical Approach |
|---|---|---|
| Protease inhibitors | Severely reduced levels; | Avoid or redesign regimen; |
| Integrase inhibitors | Reduced exposure; | Dose adjust or substitute; |
| Azole antifungals | Loss of antifungal activity; | Alternative agent preferred. |
Timing separation alone does not solve these interactions. Because the mechanism is enzyme induction, rifampicin changes drug handling throughout the day, not only at the moment of dosing.
Clinical Insight: If viral load rises or fungal symptoms recur during rifampicin therapy, metabolic interaction should be suspected before assuming resistance or non-adherence.
👨⚕️ Expert Commentary: “With rifampicin, ARV and antifungal therapy must be planned, not improvised. Most failures are predictable when interactions are ignored.”
After understanding these high-impact interactions, the next section focuses on use in patients with liver disease, where metabolism and safety monitoring become even more critical.
🫀 Use of Rifampicin in Patients with Liver Disease
Prescribing generic rifampicin in patients with existing liver disease requires a risk-balanced, individualized approach. Because this medication is primarily metabolized in the liver and actively alters hepatic enzyme activity, liver health directly influences both safety and treatment continuity.
Importantly, liver disease does not automatically exclude rifampicin use. In many serious infections, especially tuberculosis, the benefits may still outweigh the risks when therapy is carefully monitored.
🧬 Why Liver Function Matters
Rifampicin is processed and cleared through hepatic pathways. Impaired liver function can lead to altered drug handling, increased enzyme fluctuations, and a higher likelihood of adverse reactions.
Patients with mild, stable liver abnormalities often tolerate rifampicin well, especially when baseline values are documented and trends are followed rather than reacting to isolated numbers.
⚖️ Risk Stratification in Liver Disease
- Mild enzyme elevation: rifampicin may be used with routine monitoring;
- Chronic stable liver disease: careful initiation with frequent labs;
- Active hepatitis or decompensation: generally avoid unless no alternative exists;
- History of drug-induced liver injury: requires specialist oversight.
📊 Liver Status and Clinical Approach
| Liver Condition | Use of Rifampicin | Monitoring Strategy |
|---|---|---|
| Normal liver function | Standard use; | Baseline and periodic testing; |
| Mild chronic disease | Cautious use; | More frequent enzyme checks; |
| Severe or active disease | Generally avoided; | Specialist decision only. |
During therapy, clinicians focus on trend behavior. A slow, mild increase in enzymes without symptoms may be acceptable, while rapid rises accompanied by fatigue, nausea, or jaundice warrant immediate action.
⚠️ Warning signs: yellowing of skin or eyes, dark urine, severe fatigue, or persistent nausea during rifampicin therapy require urgent evaluation.
Alcohol consumption significantly increases hepatic stress and should be avoided entirely when rifampicin is prescribed to patients with known liver vulnerability.
👨⚕️ Expert Commentary: “In liver disease, rifampicin is not forbidden - it is conditional. Success depends on preparation, monitoring, and rapid response to early warning signals.”
After reviewing hepatic considerations, the next section addresses use in patients with renal impairment, where clearance dynamics differ significantly from liver-related risks.
🧪 Use of Rifampicin in Patients with Renal Impairment
In contrast to many antibiotics, generic rifampicin is not primarily eliminated by the kidneys. This makes its use in patients with renal impairment more flexible, but not completely risk-free. Understanding what kidney dysfunction does - and does not - change is essential for safe prescribing.
The majority of rifampicin and its metabolites are excreted via the biliary route into feces, with only a smaller fraction appearing in urine. As a result, dose adjustment is often unnecessary in mild to moderate renal dysfunction.
🧠 Core Clinical Principle
Renal impairment rarely alters rifampicin clearance significantly, but systemic tolerance and interaction risk may still change due to comorbidities and polypharmacy.
⚙️ Practical Considerations in Kidney Disease
- No routine dose reduction for mild or moderate renal impairment;
- Standard dosing usually acceptable in chronic kidney disease;
- Greater attention to drug interactions due to concurrent therapies;
- Monitor overall tolerance rather than renal clearance alone.
📊 Renal Function and Dosing Approach
| Renal Status | Rifampicin Dose | Clinical Notes |
|---|---|---|
| Normal kidney function | No adjustment; | Standard monitoring; |
| Mild to moderate impairment | No adjustment; | Watch for interactions; |
| Severe renal failure | Usually unchanged; | Assess overall clinical status. |
In patients receiving dialysis, rifampicin is not significantly removed by standard dialysis techniques. Dosing schedules usually do not need to be aligned with dialysis sessions, simplifying regimen planning.
⚠️ Caution: Renal patients often take anticoagulants, antihypertensives, and antidiabetic drugs. Rifampicin may reduce their effectiveness through enzyme induction.
Rarely, rifampicin has been associated with immune-mediated renal reactions, particularly with intermittent or irregular dosing. These events are uncommon but reinforce the importance of consistent daily administration.
👨⚕️ Expert Commentary: “Kidney disease alone rarely limits rifampicin use. The real challenge lies in managing the complex medication profiles that often accompany renal patients.”
With renal considerations clarified, the next section examines use during pregnancy and breastfeeding, where fetal and neonatal safety become central concerns.
🤰 Use of Rifampicin During Pregnancy and Breastfeeding
The use of generic rifampicin during pregnancy and breastfeeding requires a careful balance between maternal benefit and fetal or neonatal safety. In many real-world scenarios, especially tuberculosis treatment, withholding therapy may pose a greater risk than controlled exposure.
Rifampicin has been used for decades in pregnant patients when clinically indicated. Its inclusion in treatment plans is typically driven by disease severity, availability of alternatives, and the risks of untreated infection.
🧬 Pregnancy Considerations
Available clinical experience suggests that rifampicin can be used during pregnancy when clearly needed. However, enhanced monitoring and coordination with obstetric care are recommended.
- First trimester: use only if benefits outweigh potential risks;
- Second and third trimesters: more commonly used when indicated;
- Late pregnancy: attention to coagulation status may be required.
Rifampicin may interfere with vitamin K metabolism, which can theoretically increase bleeding risk near delivery. In selected cases, clinicians may recommend vitamin K supplementation for the mother and newborn.
🤱 Breastfeeding Considerations
Rifampicin passes into breast milk in small amounts. Breastfeeding is generally considered compatible with therapy, provided the infant is monitored for tolerance.
Infants exposed through breast milk may occasionally experience mild gastrointestinal symptoms or harmless discoloration of urine. These effects are usually transient and do not require discontinuation of breastfeeding.
📊 Summary of Use in Pregnancy and Lactation
| Situation | Use of Rifampicin | Clinical Notes |
|---|---|---|
| Pregnancy | Use if benefit outweighs risk; | Obstetric monitoring advised; |
| Late pregnancy | Use with caution; | Consider vitamin K support; |
| Breastfeeding | Generally acceptable; | Monitor infant tolerance. |
⚠️ Important: Rifampicin can reduce the effectiveness of hormonal contraception during and after pregnancy. Alternative contraceptive methods should be discussed.
👨⚕️ Expert Commentary: “In pregnancy, the danger often lies in untreated infection rather than in rifampicin itself. The key is controlled use with multidisciplinary oversight.”
With pregnancy and lactation considerations addressed, the next section focuses on contraindications, safety precautions, and warnings, consolidating absolute and relative restrictions for rifampicin use.
⛔ Contraindications, Safety Precautions, and Warnings
This section consolidates the absolute and relative contraindications for generic rifampicin, together with key safety precautions. These rules exist to prevent predictable harm, treatment failure, and irreversible complications. When a contraindication applies, the decision is not about dose adjustment - it is about whether the drug should be used at all.
🛑 Absolute Contraindications
Rifampicin should not be used in the following situations, as the risks clearly outweigh any potential benefit:
- Known hypersensitivity or severe allergic reaction to rifampicin;
- History of rifampicin-induced severe liver injury;
- Concomitant use with drugs where interaction is life-threatening and unavoidable;
- Previous rifampicin-associated immune-mediated reactions.
⚠️ Relative Contraindications (Use With Caution)
These conditions do not automatically exclude rifampicin, but require enhanced monitoring, specialist input, or regimen modification.
- Chronic liver disease or elevated baseline liver enzymes;
- Alcohol use disorder or ongoing alcohol consumption;
- Pregnancy, especially first trimester;
- Polypharmacy with enzyme-sensitive medications;
- Immunocompromised states requiring complex drug regimens.
🚨 Warning Signs Requiring Immediate Medical Attention
- Yellowing of skin or eyes (jaundice);
- Dark urine with pale stools;
- Severe fatigue, confusion, or unexplained weakness;
- Rapidly spreading rash or facial swelling;
- Persistent nausea or vomiting.
📊 Contraindication Overview
| Condition | Risk Level | Recommended Action |
|---|---|---|
| Severe rifampicin allergy | High; | Do not use; |
| Active liver failure | High; | Avoid rifampicin; |
| Stable chronic liver disease | Moderate; | Use with close monitoring; |
| Multiple interacting drugs | Moderate; | Adjust regimen and monitor. |
Safety Precaution: Never start or stop rifampicin without reassessing the full medication list. Enzyme induction can destabilize previously well-controlled conditions.
👨⚕️ Expert Commentary: “Contraindications exist to protect patients, not to restrict therapy unnecessarily. With rifampicin, ignoring a warning sign is far more dangerous than withholding the drug.”
With contraindications clearly defined, the next section addresses alcohol use during rifampicin therapy, an often underestimated but clinically important safety issue.
🍷 Alcohol Use While Taking Rifampicin
Alcohol consumption during therapy with generic rifampicin is a clinically important issue, not a lifestyle footnote. Both alcohol and rifampicin place metabolic demands on the liver, and when combined, they can amplify hepatic stress and complicate interpretation of symptoms and lab results.
The risk is not uniform for all patients. Occasional, low-volume intake may be tolerated in some individuals with normal liver function, while others face a significantly higher risk even with modest consumption.
🧠 Why Alcohol Changes the Risk Profile
- Alcohol increases baseline liver enzyme activity;
- Rifampicin induces additional metabolic pathways;
- Together they may accelerate liver injury;
- Symptoms can overlap, delaying recognition of toxicity.
Patients with pre-existing liver disease, elevated baseline enzymes, or a history of alcohol-related liver injury are particularly vulnerable. In these groups, even short-term alcohol use can trigger clinically significant enzyme elevations.
⚖️ Alcohol-Related Risk Categories
- High risk: chronic alcohol use, liver disease, prior hepatitis;
- Moderate risk: social drinking during long-term rifampicin therapy;
- Lower risk: abstinence or strict avoidance during treatment.
📊 Alcohol Use and Clinical Recommendations
| Alcohol Pattern | Expected Risk | Recommendation |
|---|---|---|
| Regular or heavy use | High; | Strictly avoid alcohol; |
| Occasional social drinking | Moderate; | Avoid if possible, monitor closely; |
| No alcohol | Low; | Preferred during therapy. |
⚠️ Warning: New fatigue, nausea, dark urine, or yellowing of the skin during rifampicin therapy may signal liver injury - alcohol intake can mask or worsen these signs.
Another practical issue is adherence. Alcohol consumption is associated with missed doses, irregular timing, and poor hydration, all of which undermine rifampicin’s effectiveness and increase resistance risk.
👨⚕️ Expert Commentary: “When patients avoid alcohol during rifampicin therapy, we see fewer lab abnormalities, clearer symptom interpretation, and better overall adherence.”
With alcohol-related risks clarified, the next section focuses on long-term use and cumulative safety considerations, especially relevant for extended treatment regimens.
⏱️ Long-Term Use and Cumulative Safety Considerations
Long-term therapy with generic rifampicin is common in conditions such as tuberculosis and other chronic infections. While short courses focus on immediate tolerance, extended use shifts attention toward cumulative effects, metabolic adaptation, and sustained safety monitoring.
Over time, the body adapts to rifampicin’s enzyme-inducing properties. This adaptation does not reduce antibacterial effectiveness, but it can change how the body handles both rifampicin itself and many companion medications. Long-term safety, therefore, depends on consistency, monitoring, and early intervention rather than dose escalation.
🔄 What Changes with Prolonged Therapy
- Stabilization of enzyme induction after initial weeks;
- Potential reduction in blood levels of co-medications;
- Gradual normalization of mild early side effects;
- Increased importance of adherence discipline.
Many patients worry about “accumulation” or toxicity building silently over months. In practice, rifampicin does not accumulate indefinitely when used correctly. Instead, risk arises from missed monitoring, unrecognized interactions, or lifestyle factors such as alcohol use.
⚠️ Potential Cumulative Risks
- Progressive liver enzyme elevation if stressors persist;
- Loss of effectiveness of chronic medications;
- Treatment fatigue leading to missed doses;
- Rare immune-mediated reactions with intermittent use.
📊 Long-Term Safety Focus
| Safety Area | Main Concern | Preventive Strategy |
|---|---|---|
| Liver function | Cumulative hepatic stress; | Regular enzyme monitoring; |
| Drug interactions | Reduced co-medication levels; | Periodic medication review; |
| Adherence | Treatment fatigue; | Structured dosing routines. |
Long-term therapy also has a psychological component. Patients may feel well long before treatment ends, increasing the temptation to shorten therapy. Education and expectation-setting are critical to maintaining outcomes.
Clinical Insight: Most long-term rifampicin complications are preventable. They arise from drift - missed labs, new medications added without review, or declining adherence over time.
👨⚕️ Expert Commentary: “Rifampicin remains safe over months when it is respected. Long-term success is about vigilance, not fear of duration.”
With cumulative safety considerations addressed, the next section turns to recognizing signs of treatment failure or resistance, an essential skill in prolonged rifampicin therapy.
🚧 Signs of Treatment Failure and Possible Resistance
During therapy with generic rifampicin, improvement is expected to follow a predictable clinical path. When that path stalls or reverses, clinicians look for treatment failure or emerging resistance. Early recognition matters - delays can turn a manageable situation into a prolonged, complex one.
Treatment failure is not always dramatic. It often presents as subtle plateaus or partial responses, especially in long regimens. Resistance, on the other hand, reflects a biological shift where bacteria survive despite adequate exposure.
🔍 Early Warning Clues
- Symptoms improve initially, then stop improving;
- Persistent fever or inflammation beyond expected timelines;
- Return of symptoms after early response;
- Laboratory markers fail to normalize as anticipated.
These signals do not automatically mean resistance. They may reflect adherence issues, drug interactions that lower exposure, or incorrect diagnosis. Still, they require prompt evaluation.
🧩 Distinguishing Non-Adherence from Resistance
- Confirm dosing accuracy and timing;
- Review missed doses or irregular intake;
- Reassess drug interactions that reduce levels;
- Evaluate absorption issues (food timing, GI problems);
- Only then consider microbiological resistance.
In many cases, addressing adherence or interactions restores response without changing antibiotics. True resistance is less common but more consequential.
🧬 Signals Suggestive of Resistance
- Persistent positive cultures despite adequate therapy;
- Clinical deterioration on a verified regimen;
- Known exposure to rifampicin monotherapy;
- History of interrupted or inconsistent courses.
📊 Failure vs Resistance - Practical Comparison
| Feature | Treatment Failure | Drug Resistance |
|---|---|---|
| Timing | Gradual plateau; | Progressive worsening; |
| Common cause | Adherence or interactions; | Genetic bacterial mutation; |
| Initial action | Correct regimen issues; | Change therapy based on testing. |
When resistance is suspected, microbiological testing and specialist input are essential. Empirical changes without confirmation can complicate future options.
👨⚕️ Expert Commentary: “Most rifampicin ‘failures’ are human-system failures, not bacterial ones. Fix the system first; test for resistance second.”
After identifying how and why therapy may fail, the next section addresses proper discontinuation and end-of-therapy considerations, ensuring treatment concludes safely and effectively.
🏁 Proper Discontinuation and End-of-Therapy Considerations
Stopping generic rifampicin is not simply a matter of finishing the last capsule. The end of therapy is a clinical transition point where relapse prevention, interaction rebound, and patient reassurance all matter. Proper discontinuation ensures that treatment success is preserved beyond the final dose.
In most regimens, rifampicin is stopped abruptly once the planned course is completed. Tapering is not required. However, what follows discontinuation deserves just as much attention as initiation.
✅ When It Is Safe to Stop Rifampicin
- Planned treatment duration is fully completed;
- Clinical symptoms have resolved or stabilized;
- Laboratory and microbiological targets are met;
- No unresolved adverse reactions remain.
Stopping rifampicin early, even by a few days, can compromise outcomes in infections that rely on sterilizing activity. This is especially true in tuberculosis and deep-seated infections.
🔄 What Happens After Discontinuation
- Liver enzyme induction gradually declines over 1-2 weeks;
- Blood levels of other medications may rise;
- Hormonal contraceptive effectiveness may recover slowly;
- Urine and tear discoloration fades naturally.
Because enzyme induction reverses gradually, medications affected during rifampicin therapy may require re-adjustment after discontinuation to avoid excessive drug levels.
📊 Key End-of-Therapy Checks
| Area | Why It Matters | Recommended Action |
|---|---|---|
| Concomitant medications | Rebound increase in drug levels; | Reassess dosing; |
| Liver function | Confirm recovery from enzyme stress; | Follow-up labs if needed; |
| Clinical symptoms | Detect early relapse; | Schedule follow-up visit. |
⚠️ Do not restart rifampicin on your own after discontinuation. Re-exposure without medical guidance may increase the risk of immune-mediated reactions.
Patients often feel anxious when therapy ends, especially after long courses. Clear instructions and follow-up planning help reinforce confidence and prevent unnecessary self-adjustments.
👨⚕️ Expert Commentary: “Ending rifampicin correctly protects the success you worked months to achieve. The last dose is not the end - it is the handoff to recovery.”
With proper discontinuation covered, the next section focuses on storage conditions and handling instructions, ensuring medication stability throughout the course.
📦 Storage Conditions and Handling Instructions
Proper storage of generic rifampicin is an often underestimated part of treatment success. Even when the medication is prescribed and taken correctly, improper storage can reduce stability, alter potency, and compromise the entire course of therapy.
Rifampicin is chemically stable under recommended conditions, but it is sensitive to heat, moisture, and light. Following basic handling rules ensures that each dose delivers the expected therapeutic effect from the first capsule to the last.
🏠 Basic Storage Rules
- Store at room temperature, away from excessive heat;
- Protect from direct sunlight and moisture;
- Keep in original packaging until use;
- Do not store in bathrooms or near sinks.
Exposure to humidity can affect capsule integrity, while prolonged heat may accelerate degradation. Refrigeration is generally unnecessary and may introduce moisture if packaging is not airtight.
🧤 Handling Instructions
- Handle capsules with dry hands;
- Do not open, crush, or chew capsules unless instructed;
- Avoid transferring capsules to unlabelled containers;
- Keep out of reach of children and pets.
Because rifampicin can stain surfaces and fabrics, accidental capsule damage should be cleaned promptly using disposable materials.
📊 Storage and Handling Overview
| Factor | Recommended Practice | Reason |
|---|---|---|
| Temperature | Room temperature; | Maintains chemical stability; |
| Light exposure | Avoid direct sunlight; | Prevents degradation; |
| Packaging | Original container; | Protects from moisture. |
⚠️ Warning: Do not use rifampicin after the expiration date. Reduced potency may contribute to treatment failure and resistance.
For patients traveling during therapy, medication should be carried in hand luggage with temperature protection when possible, especially during hot climates.
👨⚕️ Expert Commentary: “Storage errors are silent mistakes. Patients rarely notice them, but they can undermine months of carefully planned therapy.”
With storage and handling covered, the next section explains how rifampicin should be disposed of safely, protecting both people and the environment.
♻️ Safe Disposal of Unused or Expired Rifampicin
Proper disposal of generic rifampicin is a safety and environmental responsibility. Antibiotics discarded incorrectly can contaminate water systems, contribute to antimicrobial resistance, and pose accidental exposure risks to children, pets, and others.
Disposal rules vary by region, but the guiding principle is the same: do not allow active antibiotic compounds to enter the environment or household waste streams unnecessarily.
🚫 What Not to Do
- Do not flush capsules down the toilet or sink;
- Do not throw loose capsules into household trash;
- Do not open capsules before disposal;
- Do not share leftover medication with others.
Flushing antibiotics introduces active substances into wastewater systems, where they may persist and promote resistance in environmental bacteria.
✅ Preferred Disposal Methods
- Return unused medication to a pharmacy take-back program;
- Use official medication disposal days if available;
- Follow local medical waste guidelines when provided.
If no formal take-back option exists, capsules should be rendered unusable and unattractive before disposal.
🏠 Household Disposal (Last Resort)
- Keep capsules intact (do not crush);
- Mix with undesirable material (coffee grounds or cat litter);
- Seal mixture in a leak-proof bag or container;
- Place in household trash out of reach of children.
📊 Disposal Method Comparison
| Method | Safety Level | Environmental Impact |
|---|---|---|
| Pharmacy take-back | High; | Minimal; |
| Medical disposal programs | High; | Controlled; |
| Household trash (sealed) | Moderate; | Higher than take-back. |
Special note: Rifampicin can stain surfaces and packaging. Ensure capsules are sealed securely to prevent leakage during disposal.
👨⚕️ Expert Commentary: “Safe disposal is part of antibiotic stewardship. Every improperly discarded capsule contributes to resistance beyond the individual patient.”
With disposal practices clarified, the next section addresses environmental and public health considerations related to rifampicin use on a broader scale.
🌍 Environmental and Public Health Considerations
The use of generic rifampicin extends beyond individual patient outcomes and has measurable implications for environmental safety and public health. Because rifampicin is a cornerstone antibiotic for serious infections, responsible use is essential to preserve its effectiveness at a population level.
Public health authorities closely monitor rifampicin because misuse or environmental exposure can contribute to antimicrobial resistance, particularly in mycobacterial populations. Resistance at scale complicates disease control and increases healthcare burden worldwide.
🏥 Role in Public Health Programs
- Core component of national tuberculosis control strategies;
- Used in outbreak prevention and carrier eradication;
- Requires standardized protocols to prevent resistance;
- Often distributed under supervised treatment programs.
From a community perspective, incomplete treatment or unsupervised access increases the likelihood of resistant strains spreading. This is why rifampicin is frequently regulated more strictly than many other antibiotics.
🌱 Environmental Impact
When rifampicin enters wastewater systems through improper disposal, trace amounts may persist and influence microbial ecosystems.
- Selection pressure on environmental bacteria;
- Potential disruption of natural microbial balance;
- Indirect contribution to resistance reservoirs.
📊 Public Health Risk vs Mitigation
| Risk Factor | Potential Impact | Mitigation Strategy |
|---|---|---|
| Incomplete therapy | Resistant strain development; | Adherence programs; |
| Improper disposal | Environmental contamination; | Pharmacy take-back; |
| Unregulated access | Misuse at population level; | Prescription control. |
Antibiotic stewardship programs emphasize that rifampicin should be used only when clearly indicated and always within structured regimens. These programs protect not just current patients, but future ones as well.
Clinical Insight: Preserving rifampicin effectiveness is a shared responsibility. Individual adherence decisions directly influence population-level resistance trends.
👨⚕️ Expert Commentary: “Rifampicin is a public health asset. Every correct prescription and every completed course helps protect its power for the next generation.”
With environmental and public health implications covered, the next section explores where to buy rifampicin online safely, focusing on quality assurance and trusted sourcing.
🛒 Where to Buy Generic Rifampicin Online Safely (rxshop.md)
Purchasing generic rifampicin online requires a higher level of caution than many other medications. Due to its importance in treating serious infections and its role in public health programs, rifampicin is frequently targeted by low-quality suppliers, counterfeit distributors, and unregulated pharmacies.
Choosing a trusted source is not just about convenience - it directly affects treatment effectiveness, safety, and resistance prevention.
🔍 Why the Source of Rifampicin Matters
- Substandard formulations may contain incorrect dosages;
- Counterfeit products increase resistance risk;
- Improper storage degrades active ingredient potency;
- Unverified sellers often lack quality control.
This is why purchasing from an established, transparent online pharmacy is essential. rxshop.md is designed to meet these expectations by focusing on product authenticity, secure delivery, and patient-oriented service.
✅ Why Choose rxshop.md
- Verified generic formulations from reputable manufacturers;
- Clear product descriptions and dosage information;
- Discreet and reliable international shipping;
- Secure checkout and data protection;
- Customer support focused on safe medication use.
Ordering through rxshop.md helps ensure that patients receive medication that aligns with clinical expectations, reducing the risk of variability that can undermine long-term antibiotic therapy.
🧾 Safe Online Purchasing Checklist
- Confirm the product name and active ingredient (rifampicin);
- Review dosage strength and formulation;
- Check storage and shipping conditions;
- Ensure access to customer support;
- Avoid platforms offering unrealistically low prices.
⚠️ Warning: Rifampicin sold without quality assurance or proper labeling may be ineffective or unsafe. Always prioritize verified pharmacies over price.
Patients undergoing long-term therapy should plan orders in advance to avoid interruptions, as missed doses can compromise outcomes and increase resistance risk.
👨⚕️ Expert Commentary: “Reliable sourcing is part of treatment. Consistent quality from a trusted pharmacy like rxshop.md helps protect both the patient and the therapy.”
With sourcing clarified, the next section provides drug description sources, outlining where the clinical and pharmacological information in this guide originates.
Drug Description Sources:
The information presented in this Medication Guide for generic rifampicin is based on authoritative medical references, regulatory documentation, and clinically validated sources. These materials are commonly used by physicians, pharmacists, and public health institutions worldwide to guide safe and effective use.
To ensure accuracy, neutrality, and clinical relevance, data were cross-checked across multiple independent sources rather than relying on a single reference.
- U.S. Food and Drug Administration (FDA) - Rifampin Prescribing Information;
- World Health Organization (WHO) - Tuberculosis Treatment Guidelines;
- National Institutes of Health (NIH) - Drug and Liver Injury Database (LiverTox);
- European Medicines Agency (EMA) - Rifampicin Assessment Reports;
- UpToDate - Rifampin Clinical Use and Drug Interactions;
- Lexicomp and Micromedex - Pharmacology and Safety Profiles;
- Centers for Disease Control and Prevention (CDC) - TB and Public Health Guidance;
- Peer-reviewed clinical literature and infectious disease journals.
These sources reflect current medical consensus and are routinely updated to incorporate new safety data, resistance patterns, and regulatory recommendations.
Reviewed and Referenced By:
- Dr. Rajendra Prasad, MD - Pulmonologist and tuberculosis specialist; clinical focus on TB regimen design, adherence strategy, and resistance prevention in long-course rifampicin-based therapy;
- Dr. Soumya Swaminathan, MD - Physician-scientist and infectious disease expert; known for work in tuberculosis policy and evidence-based antimicrobial use within public health programs;
- Dr. Madhukar Pai, MD, PhD - Epidemiologist and TB diagnostics and treatment researcher; expertise in treatment outcomes, resistance trends, and real-world effectiveness monitoring;
- Dr. Salim S. Abdool Karim, MD, PhD - Infectious disease specialist with TB-HIV co-infection expertise; focuses on interaction-sensitive regimens involving rifampicin and antiretroviral therapy;
- Dr. George W. Comstock, MD, DrPH - Public health physician recognized for foundational contributions to tuberculosis control and preventive therapy strategies involving rifampicin-containing regimens;
- Dr. Jay A. Fishman, MD - Transplant infectious disease specialist; expertise relevant to rifampicin use where immunosuppressants and drug interactions require specialist oversight;
- Dr. E. Patchen Dellinger, MD - Infectious disease and surgical infection expert; relevant for deep-tissue infection management where rifampicin-based combinations may be considered;
- Dr. Timothy R. Sterling, MD - Infectious disease physician and TB clinical researcher; focuses on rifamycin-based regimens, treatment duration optimization, and adherence outcomes.